Keywords: TBI, TBI treatment, TBI patient pathway, TBI emergency treatment, TBI severity, precision medicine
What happens after a TBI? This question comes as a follow up to “Why is TBI considered a global burden?” which describes the epidemiology of TBI, populations most affected, post-traumatic disability, the impact of TBI on the quality of life, prevention measures and policy recommendations regarding TBI.
According to the Global Burden of Disease study published in 2016, TBI has an incidence of over 25 million cases yearly and a prevalence of over 55 million [1]. Nevertheless, one must consider that a certain number of TBI victims do not reach medical care, leading to an underestimation of the actual rates [2].
What is TBI treatment?
TBI is characterized by heterogeneity. The causes, mechanisms, consequences, type of progression, and outcomes present significant variability, thus making the management and treatment of TBI complex and heterogeneous.
The pathogenesis of TBI is a cumulation of complicated and intricated processes that represent the results of the causative TBI. Following the TBI, primary and secondary injuries lead to various neurological and non-neurological alterations that result in the heterogeneous clinical presentation of the patients, with the associated disorders of consciousness ranging from mild to profound coma or death [2].
The role of TBI treatment and management is to minimize the consequences related to the primary injury, consisting of the external force attributed to the brain, and to prevent, as much as possible, the secondary injuries that usually appear after the primary injury. The secondary injuries are found on molecular and chemical levels. The activation of an inflammatory cascade leads to continuous lesions resulting in neuronal death and blood-brain barrier disruption. Fortunately, the injury phase is followed by the neurorecovery phase, which consists of anatomic-functional reorganization of the affected brain tissue [2].
TBI Severity
Currently, the classification of TBI is not sufficiently detailed to ensure personalized treatment for the patients. Furthermore, there are no established criteria for depicting quality care in TBI [3]. As traumatic brain injury (TBI) is often encountered in certain populations (e.g. military personnel), leading to it being often called the ‘silent epidemic’ of modern times, understanding the TBI severity and options for treatment is of utmost importance [4–6].
To date, the most used classification regarding the severity of TBI defining mild, moderate, and severe lesions, is based on the elements described in the graphic below:

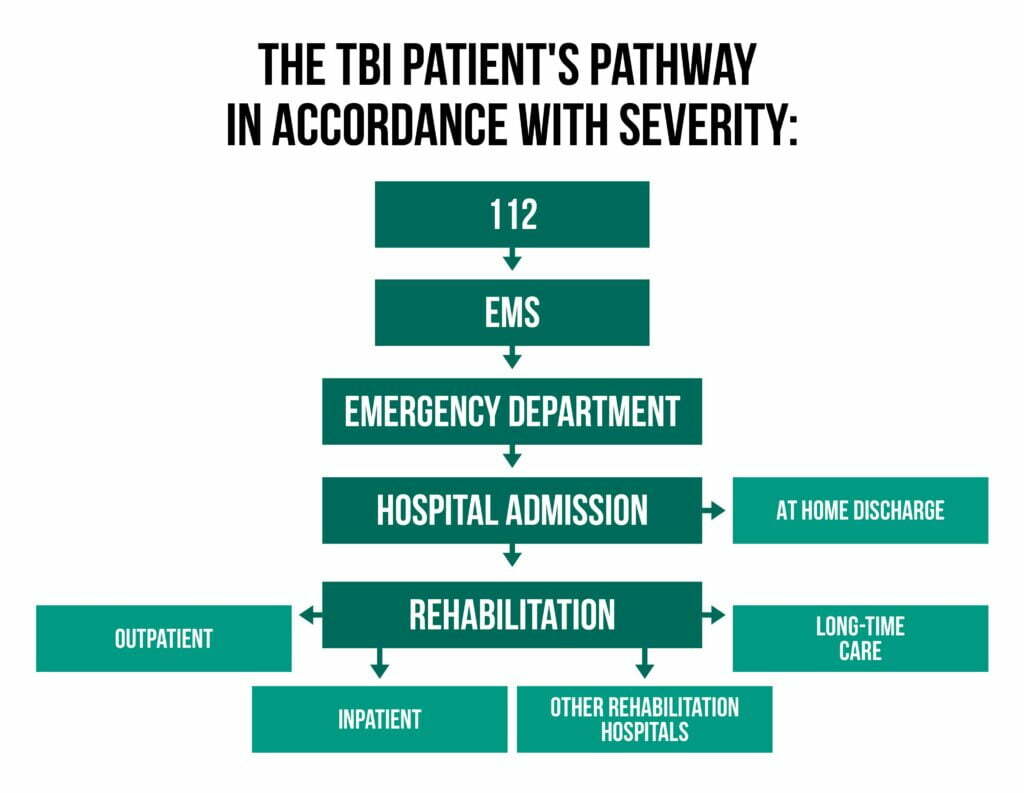
The TBI patient’s pathway in accordance with severity is represented in the following graphic:
What is being done?
The content inside the cranial cavity comprises the brain tissue, cerebrospinal fluid, and blood. These are all altered during a TBI, the loss of a balance among them leading further to different neurological deficits and increased intracranial pressure.
TBI treatment requires adequate management of the heterogenous consequences (regarding the type, the area of the brain involved, and the volume affected) to ensure the best possible outcomes [2].
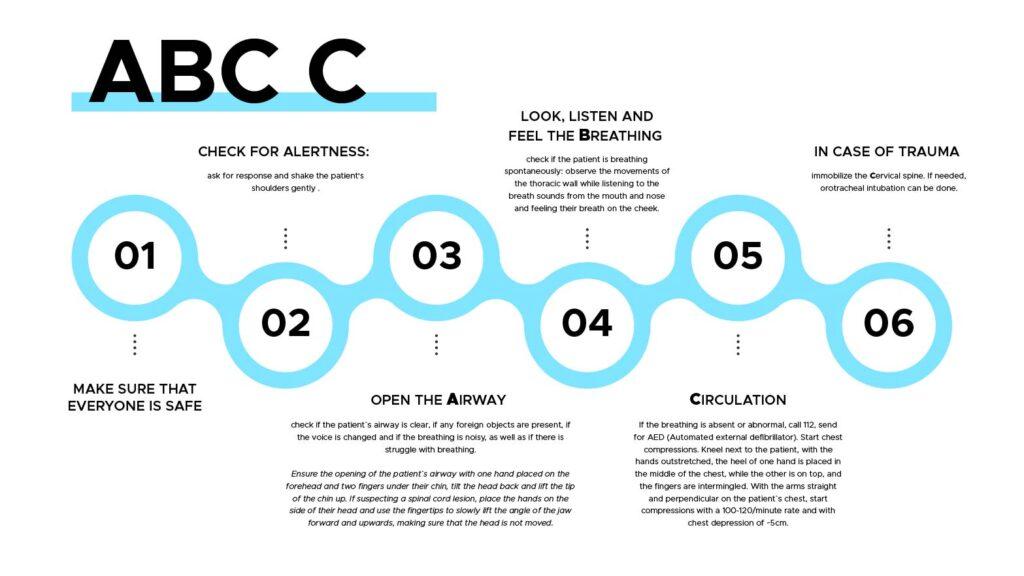
The emergency treatment of moderate and severe TBI patients focuses on stabilizing the patient’s vital functions, in other words assuring that the patient is being kept alive. The treatment begins in the pre-hospital phase and is described below:
ABC C :
(1) Make sure that everyone is safe
(2) Check for alertness: ask for response and shake the patient’s shoulders gently .
(3) Open the Airway – check if the patient’s airway is clear, if any foreign objects are present, if the voice is changed and if the breathing is noisy, as well as if there is struggle with breathing.
Ensure the opening of the patient’s airway with one hand placed on the forehead and two fingers under their chin, tilt the head back and lift the tip of the chin up. If suspecting a spinal cord lesion, place the hands on the side of their head and use the fingertips to slowly lift the angle of the jaw forward and upwards, making sure that the head is not moved.
(4) Look, listen and feel the Breathing – check if the patient is breathing spontaneously: observe the movements of the thoracic wall while listening to the breath sounds from the mouth and nose and feeling their breath on our cheek;
(5) Circulation – If the breathing is absent or abnormal, call 112, send for AED (Automated external defibrillator). Start chest compressions. Kneel next to the patient, with the hands outstretched, the heel of one hand is placed in the middle of the chest, while the other is on top, and the fingers are intermingled. With the arms straight and perpendicular on the patient’s chest, start compressions with a 100-120/minute rate and with chest depression of ~5cm.
(6) In case of trauma immobilize the Cervical spine [7, 8]. If needed, orotracheal intubation can be done.
Additional measures include:
– Oxygenation (administering O2 in all TBI patients)
– Blood pressure control (avoiding hyper- and hypotension)
These are usually followed by the in-hospital care management of TBI, which is described in the graphic below:
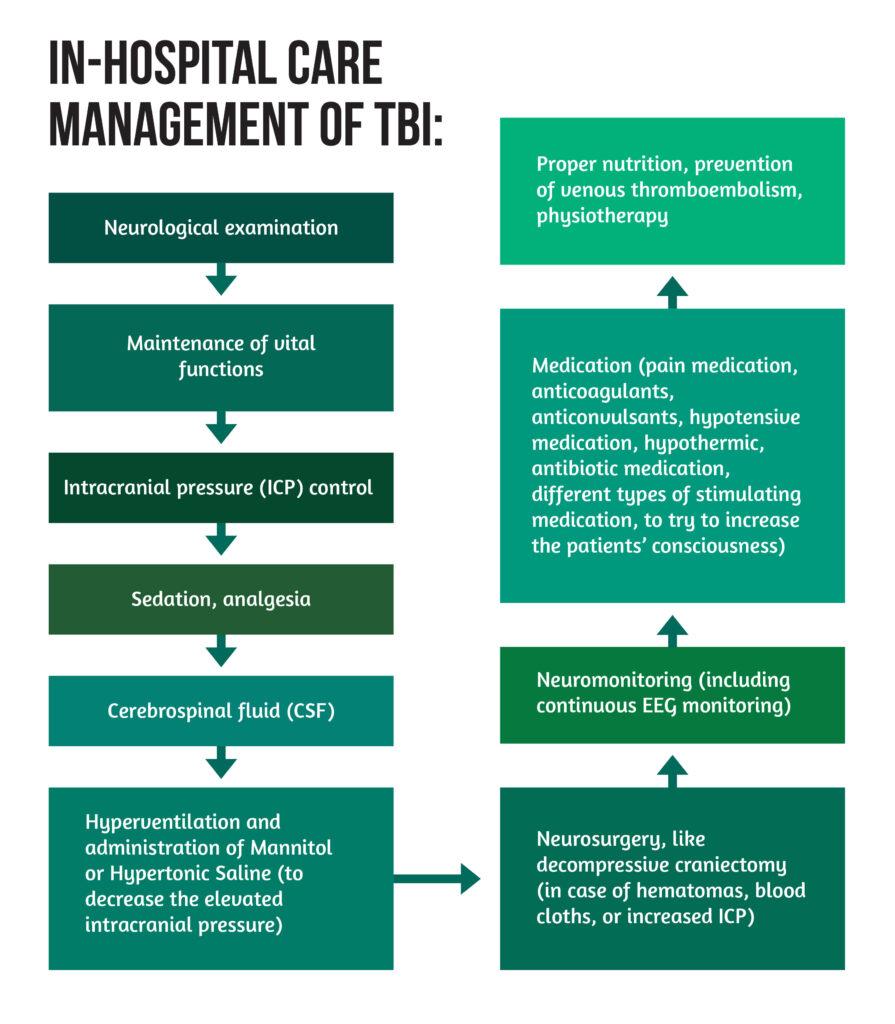
** CSF = Cerebrospinal Fluid ; ICP = intracranial pressure ; EEG = electroencephalogram
Unfortunately, because part of the pathological mechanisms are still unknown and TBI is characterized by substantial heterogeneity, no “golden standard” treatment currently exists [3].
What happens after a TBI? Why do patient outcomes differ between centers?
Several studies have shown significant differences regarding the outcome of TBI patients between centers, countries, regions, and access to resources. As mentioned above, TBI treatment is based mainly on ensuring physiological conditions for TBI patients. Although, this approach is insufficient because it does not offer personalized patient care in accordance with the severity, consequences of TBI, and mechanisms affecting outcomes [3].
Studies conducted on an international level have shown the quality of care mirrored in the patients’ outcomes. In addition, these have indicated significant differences between hospitals regarding outcomes, with specialized trauma centers having better results for severely affected patients due to the intensive therapy and algorithm-based management of patients [3].
The significant differences in outcomes come secondary to:
- the context of limited treatment possibilities for TBI resulting in different ways of TBI management;
- translational research findings (primary research) emphasizing that the shift to clinical care is difficult and time-consuming;
- the existing guidelines not being implemented accordingly;
- the availability of resources influencing the organization of trauma systems and the implementation of guidelines, patient pathways, and overall care.
The lack of quality criteria for the care of TBI patients affects its assessment and the patient’s outcome overall. The solution is to collect TBI data and integrate the available evidence into local guidelines that are adapted to local conditions. Moreover, the data could prove an important asset in cost-effectiveness studies potentially leading to the allocation of resources in accordance to needs [3].
From bench to bedside in TBI : Research
Despite the new types of research and the enhanced understanding of the various mechanisms of injury and patient care, the available evidence used for different parts of TBI guidelines does not have complete reliability. Nevertheless, the use of guidelines and algorithms developed on evidence-based treatments and management of TBI have led to improvement in outcomes. These are usually based on the continuously upgraded search of systematic reviews and meta-analyses from the existing literature. Furthermore, improvement in the pre-hospital phase and intensive care led to better outcomes [6].
When discussing the classical types of research, the randomized clinical trials used for treatment research of TBI have multiple disadvantages. The selection of patients is not always representative for the entire population due to the difficulty of gathering a sample of patients with identical lesions. If they are being selected by the severity of TBI (as mentioned above), failing to consider the mechanisms, age, comorbidities, and other variables/factors, leads to significant errors.
For these considerations a better management and treatments for TBI patients can be achieved through the use of precision medicine, which comprises of:
- detailed characterization of patients
- diligent monitoring of TBI
- use of artificial intelligence as an addon for clinical decision making
- MRI (Magnetic Resonance Imaging)
- assessment of blood biomarkers (e.g., S100B)
- genetics evaluations
Furthermore, there is a dire need to strive for a more detailed assessment of disability in patients, as well as for cross-referencing the effectiveness of different hospitals in treating TBI patients [3].
References
- GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016 [published correction appears in Lancet Neurol. 2021 Dec;20(12):e7]. Lancet Neurol. 2019;18(1):56-87. doi:10.1016/S1474-4422(18)30415-0
- Galgano M, Toshkezi G, Qiu X, Russell T et al. Traumatic Brain Injury: Current Treatment Strategies and Future Endeavors. Cell Transplant. 2017;26(7):1118-1130. doi:10.1177/0963689717714102
- Traumatic Brain Injury Fact sheets and Policy brief CENTER-TBI. Retrieved from: https://www.center-tbi.eu/files/news/21571f81-20b8-4860-a3dd-1f6e27d02b3d.pdf
- O’Neil ME, Carlson K, Storzbach D, et al. Complications of Mild Traumatic Brain Injury in Veterans and Military Personnel: A Systematic Review [Internet]. Washington (DC): Department of Veterans Affairs (US); 2013 Jan. Table A-1, Classification of TBI Severity. Available from: https://www.ncbi.nlm.nih.gov/books/NBK189784/table/appc.t1/
- US Department of Health and Human Services, Office of Communications, 24.11.2020, What are the treatments for traumatic brain injury (TBI)?, accessed on 6.4.2022, https://www.nichd.nih.gov/health/topics/tbi/conditioninfo/treatment
- Dash HH, Chavali S. Management of traumatic brain injury patients. Korean J Anesthesiol. 2018;71(1):12-21. doi:10.4097/kjae.2018.71.1.12
- Olasveengen TM, Semeraro F, Ristagno G, Castren M, Handley A, Kuzovlev A, Monsieurs KG, Raffay V, Smyth M, Soar J, Svavarsdottir H, Perkins GD. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation. 2021 Apr;161:98-114. doi: 10.1016/j.resuscitation.2021.02.009. Epub 2021 Mar 24. PMID: 33773835.
- National Health Service, 15.03.2022, After an incident-First aid, https://www.nhs.uk/conditions/first-aid/after-an-accident/ accessed on the 11th of April 2022.




