Keywords: TBI, treatment, recovery, brain injury, therapy
Introduction | Severe TBI treatment
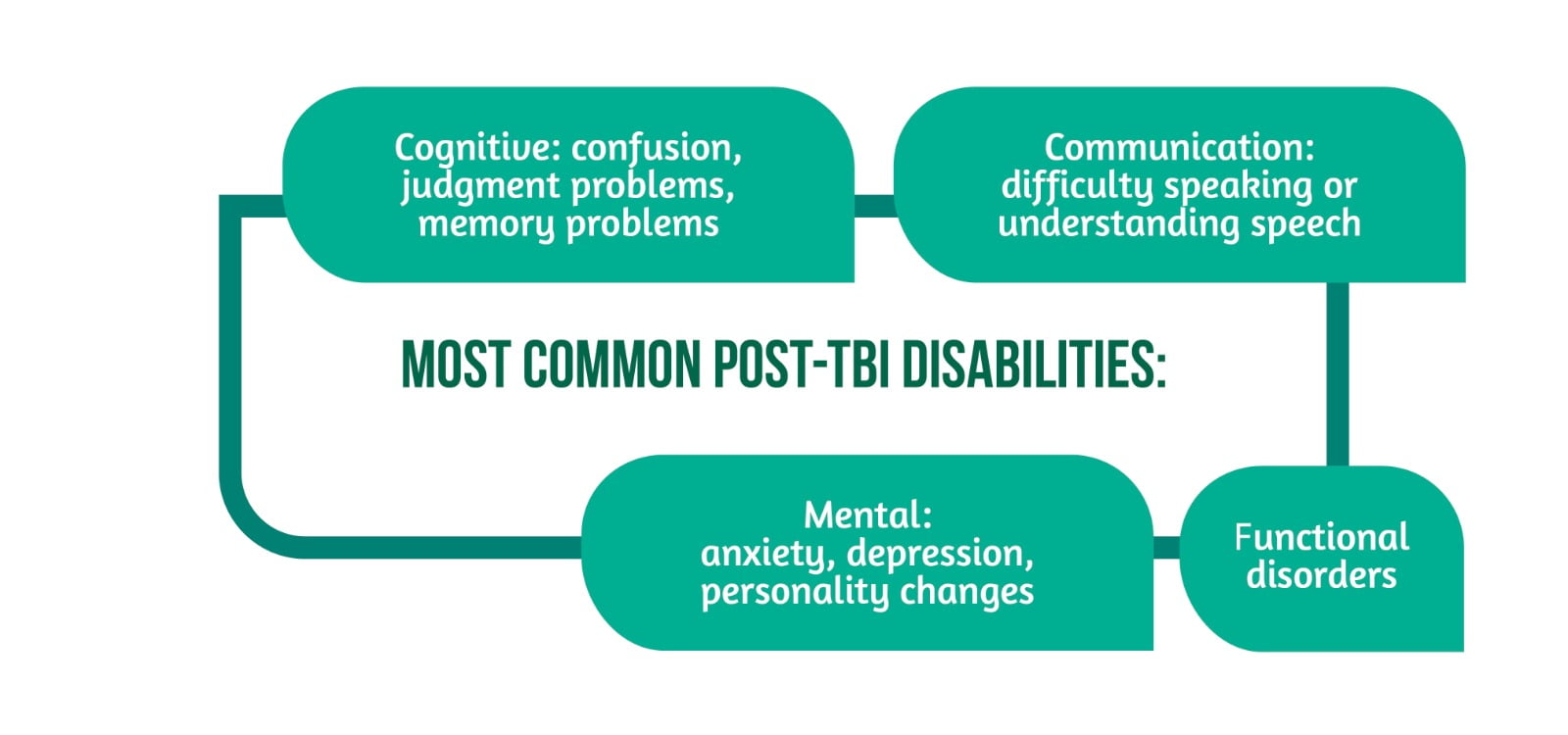
Traumatic brain injury (TBI) represents a significant problem at the global level due to the increased number of cases and the significant impact on the quality of life. Furthermore, patients with TBI present multiple disabilities, which is why they need continuous care and multiple treatments, leading to high costs for society and their families. The most common disabilities are presented in Figure 1 [1].
What is severe TBI?
TBI occurs due to the action of strong external forces on the brain tissue leading to cerebral ischemia and cell destruction. Usually, the severity of the TBI is established by calculating the GCS (Glasgow Coma Score) after the initial resuscitation of the victim. In the case of patients with severe TBI, the GCS score is lower than 9 points, and the patient is unconscious for some time, with the impossibility of responding to environmental stimuli. The alteration of the state of consciousness can have several levels [1], including:
- Coma represents a state of unconsciousness in which the patient has closed eyes and cannot respond to tactile, verbal, or painful stimuli. The patient cannot:
- be taken out of this state,
- respond to commands
- perform actions with a specific purpose.
- Vegetative state – the patient can open his eyes but is unconscious. They can respond to verbal stimuli, touch, smile, or cry, but these actions are reflexes and cannot be done voluntarily.
- Minimally conscious state – the patient experiences alternation of awareness and response to stimuli with episodes of unconsciousness. It can present with episodes in which they make simple gestures and try to communicate verbally or through gestures. Improving the state of unconsciousness specific to the coma or the vegetative state leads to the state of minimal consciousness.
- Emerged from the minimally conscious state refers to patients who can communicate consistently or learn to use at least two objects purposefully.
- The post-traumatic confusional state represents a state in which the patient regains consciousness. Still, confusion and memory disorders persist with the impossibility of forming new memories or performing purposeful actions. This condition can also be called post-traumatic amnesia. Also, the patients present behavioral disorders with increased emotional lability, agitation, impulsiveness, and physical aggression. During episodes of psychomotor agitation, patients may pull on feeding or ventilation tubes, injuring themselves [1, 2].
How is a patient with TBI treated?
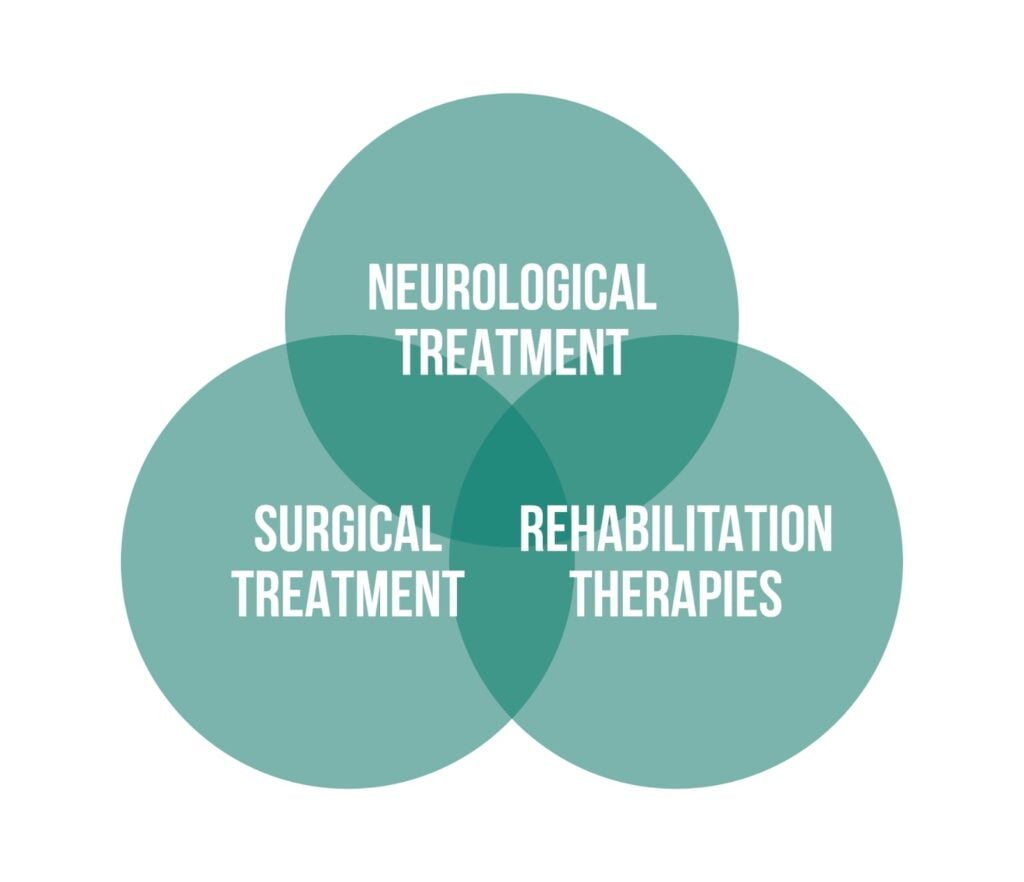
Each patient with TBI must be treated differently depending on his present injuries and preexisting comorbidities. Therefore, several treatments may be necessary for TBI patients, including those described in Figure 2.
Firstly, the victim arrives at the acute care center, and doctors will treat life-threatening conditions such as:
- airway obstruction,
- hemorrhagic shock,
- increased intracranial pressure,
- tension pneumothorax [3].
- Neurological treatment involves monitoring the patient and administering medication (anticonvulsants, diuretics, anticoagulants, antihypertensive and anti-anxiety medication) to avoid secondary injuries [1].
- Surgical treatment (e.g., repairing fractures, releasing increased intracranial pressure, or removing a hematoma). Sometimes surgical treatment is urgently needed to avoid brain tissue damage.
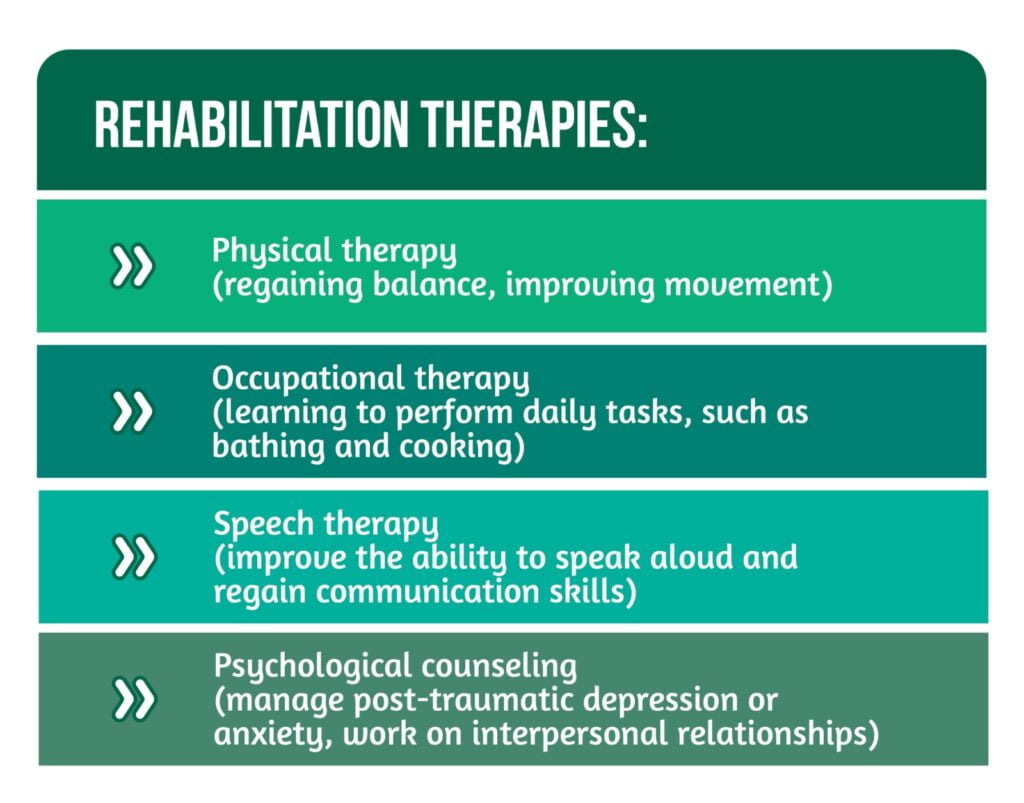
- Rehabilitation therapies help patients to regain the functions lost after a TBI. Rehabilitation begins during hospitalization and can continue throughout life in the case of patients with significant sequelae. There are several types described in Figure 3.
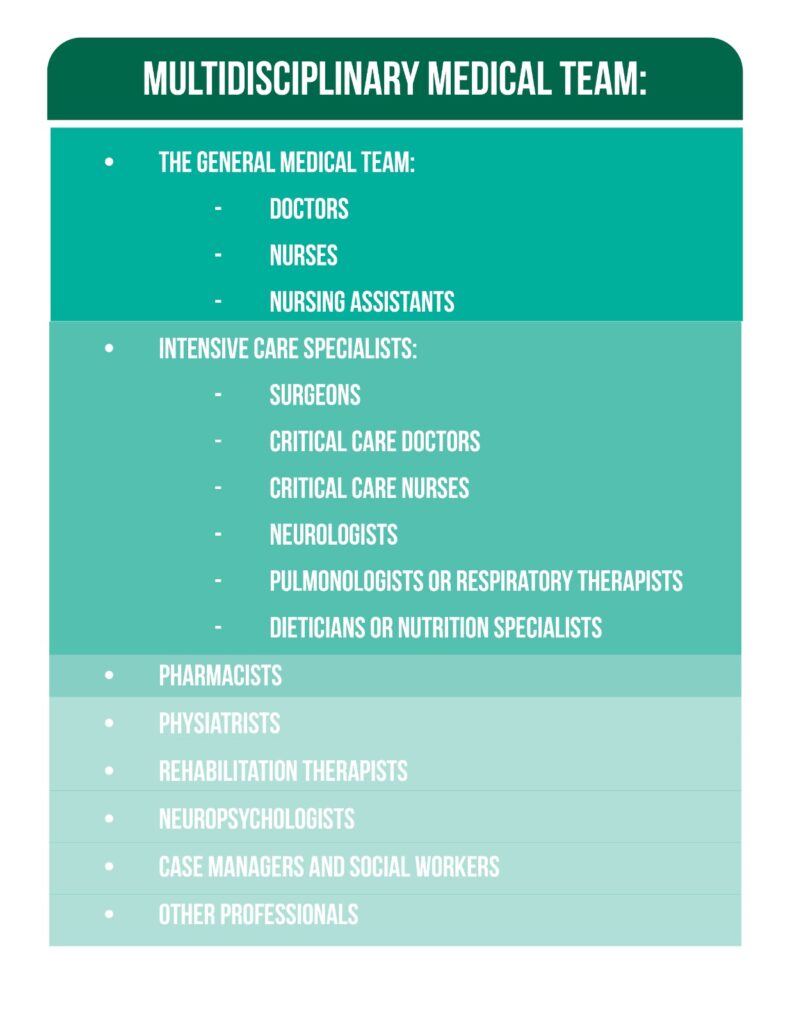
Most patients with TBI have multiple injuries and need several treatments provided by qualified medical personnel. In addition to their role in patient care, the medical staff is a source of information and support for patients and their families. The medical team should be composed of the following people:
- The general medical team– e.g., doctors, nurses, and nursing assistants who ensure the care of patients and the administration of the necessary treatments [1].
- Intensive care specialists– the team must include at least one doctor specialized in trauma care of patients with TBI and their recovery:
- Surgeons should be part of the team because the patient’s condition may worsen, requiring a surgical intervention to save his life.
- Critical care doctors treat patients who require intensive care.
- Critical care nurses help the doctor perform the procedures, administer the medication, and inform the patient’s family about his condition.
- Neurologists deal with the diagnosis and treatment of brain disorders. They examine the patient to determine the extent of the head trauma and monitor the neurological recovery.
- Pulmonologists or respiratory therapists treat respiratory problems.
- Dieticians or nutritional specialists ensure the food intake for each patient according to his energy needs.
- Pharmacists- help the doctor determine the necessary doses of the drugs, prepare some medications, and provide information about possible side effects [1].
- Physiatrists– help treat many medical problems that affect the brain, bones, muscles, joints, and tendons.
- Rehab therapists- provide a wide range of therapies (physical, occupational, respiratory, or cognitive therapy) necessary for regaining the functional abilities of patients with severe TBI and increasing their quality of life.
- Neuropsychologists- diagnose behavioral, emotional, or thinking problems after a TBI. They also have an important role in supporting and educating the patient’s family about TBI.
- Case managers and social workers- help the family with financial or health insurance information and coordinate the long-term care plan.
- Other professionals- sometimes others are needed, such as a chaplain, or patient representative, to offer emotional and spiritual support to the patient and his family [1]. (Figure 3).
Which investigations are necessary for TBI?
Paraclinical investigations are used to establish the diagnosis of TBI and the extent of brain damage, but they are essential in choosing the appropriate treatment. The following tests and procedures are used most frequently:
- Neuroimaging studies: Computed tomography (CT) and magnetic resonance imaging (MRI) are used to determine the location of the lesions and the need for surgical intervention.
- Electroencephalograms (EEG) are tests that examine the brain’s electrical activity, helping to diagnose seizures and establish the location of brain injury.
- Neurological monitoring: Intracranial pressure monitoring is necessary for TBI patients to avoid complications. It is necessary to mount a tube at the brain level connected to a device that measures the pressure, and when it is increased, it can eliminate the excess pressure. Neuromonitoring is also helpful in the case of excess cerebrospinal fluid (hydrocephalus) until a shunt is installed to drain the fluid.
- Neurological exams: Doctors try to evaluate changes in the state of consciousness, response to stimuli, and signs of purposeful movements [1].
What is expected in recovering after a severe TBI?
Establishing the prognosis in the case of patients with severe TBI is challenging for the clinician because recovery is a long process, and each person can evolve differently. Therefore, it takes a long time (weeks or months) for the doctor to be able to estimate how much the patient will recover after TBI [1].
The process of recovering the state of consciousness takes place slowly, step by step. Some patients go through all the stages of an altered state of consciousness (coma- vegetative state- minimally conscious state- emerged from a minimally conscious state- post-traumatic confusional state), noticing small improvements that appear gradually over time. The patient does not need to go through all the stages described above. Some can skip a certain stage, while others can stay in a specific state for a long time.
Post-TBI recovery is a long process. Some patients can regain consciousness a few days after the accident, while others remain unconscious for months or even years [1]. Most progress was observed in the first 6 months. As time goes by, the speed of recovery decreases, but improvements can still be observed. The recovery rate after a TBI varies from one person to another [4].
Following a moving object with the eyes is a sign of improvement in TBI patients. This sign, also called visual tracking, is one of the first behaviors that appear when the patient’s condition improves, passing to a state of minimal consciousness. The best prognosis is for patients who quickly pass from a state of coma or vegetative to a state of minimal consciousness. The correct assessment of the level of the state of consciousness is an essential step in predicting the short- and long-term outcomes and establishing the need for specialized rehabilitation [1].
Age and pre-injury health are important factors with a role in prognosis. Young patients with no previous traumas have higher chances of being able to lead independent life [4].
What can be done to help patients post-TBI?
In the case of patients with TBI, the family plays an essential role both in providing information about the previous state of the victim as well as in the recovery process [1]. Caregivers should know that:
- The doctors will ask questions about the injured person’s medication and allergies, but also about preexisting medical conditions.
- Patients with severe TBI cannot make decisions about medical treatments. These will be made by their family or by the legal decision-maker. The patient’s wish regarding resuscitation must be respected when he has a signed advance directive.
- Family members must be aware of the changes that may occur after a TBI, such as behavioral, cognitive, and psychological changes.
- Family members are very important in case of a significant event, but taking care of oneself remains a priority for caregivers.
- The family should learn how to interact with the TBI patient and be attentive to all the changes in his condition [1].
How should you interact with a TBI patient?
Some advice for interacting with TBI patients includes the following:
- After a severe TBI, patients need limited periods of stimulation alternating with rest periods. The number of visits and their duration should be limited. The medical team’s recommendations regarding what type of stimulation is suitable and the appropriate duration must be followed to favor the rehabilitation of the loved one.
- Striving to create a pleasant environment for the loved one (e.g., play their favorite music while looking at family photos, stimulate their senses).
- Communication is important in rehabilitating TBI patients, even if they cannot understand (e.g. sharing funny memories or just reading them the newspaper or a favorite book).
- Test the ability of the loved one to perform commands such as shaking hands and opening the mouth, or the ability to make eye contact.
- When the loved one regains consciousness, it is important to tell him what happened, where he is at the moment, and information about the date and time [1].
In conclusion, TBI represents a major event in every family with multiple negative consequences. A long rehabilitation period is necessary to increase the quality of life of the loved one and recover the deficits. Caring for a patient with TBI requires a lot of patience and attention to maintain individual needs. Moreover, estimating the prognosis after a severe TBI remains a challenge for the physician because each patient evolves differently, and a long period is needed to approximate this [1].
For more information about the impact of TBI visit:
- Immune response post-TBI
- How does TBI affect the functions of patients?
- Advances in TBI care and therapies
Conclusions
Traumatic Brain Injury (TBI) poses a complex challenge both medically and socially, given its varied impact on patients’ lives and the high cost of continuous care. The treatment of severe TBI is multifaceted, involving immediate and critical medical interventions, followed by long-term rehabilitation therapies. The journey from acute care to rehabilitation is characterized by a need for personalized treatment strategies, considering each patient’s specific injuries and pre-existing conditions.
The recovery process in severe TBI cases is gradual and can vary significantly from one patient to another. Progress is often most notable in the first six months post-injury, with the rate of recovery slowing down over time. However, continuous improvements are possible, and each small step forward is a significant milestone in the patient’s journey to recovery.
Family involvement is crucial in the TBI recovery process. The role of the family extends beyond providing support and care; they are integral in helping the medical team understand the patient’s pre-injury state and in making critical medical decisions. Moreover, the family must be prepared for the potential cognitive, behavioral, and psychological changes in the patient post-injury.
Interacting with a TBI patient requires a careful and informed approach. Limiting the duration and intensity of stimulation, creating a comfortable environment, and maintaining communication, even when the patient seems unresponsive, are all key to aiding their recovery. As patients regain consciousness, it’s important to reorient them and keep them informed about their situation.
In conclusion, severe TBI treatment is a long-term commitment that requires a coordinated effort from medical professionals, the patient, and their family. Each case is unique, and while the prognosis can be challenging to predict, continuous care and rehabilitation can significantly improve the patient’s quality of life. For more information on the impact of TBI, advancements in care, and therapies, further resources on immune responses post-TBI and the effects of TBI on patient functions can be consulted.
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
Bibliography
- Model Systems Knowledge Translation Center. Severe Traumatic Brain Injury: What to Expect in the Trauma Center, Hospital, and Beyond; 2017; Available from: https://msktc.org/tbi/factsheets/severe-traumatic-brain-injury.
- Marshman LAG, Jakabek D, Hennessy M, Quirk F, et al. Post-traumatic amnesia. Journal of Clinical Neuroscience. 2013;20(11):1475–81; doi: 10.1016/j.jocn.2012.11.022.
- Planas JH, Waseem M, Sigmon DF. Trauma Primary Survey. StatPearls Publishing; 2022 Available from: http://www.ncbi.nlm.nih.gov/books/NBK430800/
- the European Task Force on Disorders of Consciousness, Laureys S, Celesia GG, Cohadon F, Lavrijsen J, León-Carrión J, et al. Unresponsive wakefulness syndrome: a new name for the vegetative state or apallic syndrome. BMC Med. 2010;8(1):68; doi: 10.1186/1741-7015-8-68.