Authors: Lavinia Filip, Silvina Ilut
Keywords: concussion, children, sports, prevention, return to school
Introduction | Sports-Related Concussions in Pediatry
The term “sport-related concussion” (SRC) refers to a traumatic brain injury brought on by biomechanical forces from a hit to the head, neck, face, or body that transmits an impulsive force to the brain. The physiological causes of damage and subsequent recovery are still not completely understood. According to a recent expert consensus, studying SRC in children should be a research priority in the future because there is a knowledge gap on the effects of concussions in children and adolescents [1, 2].
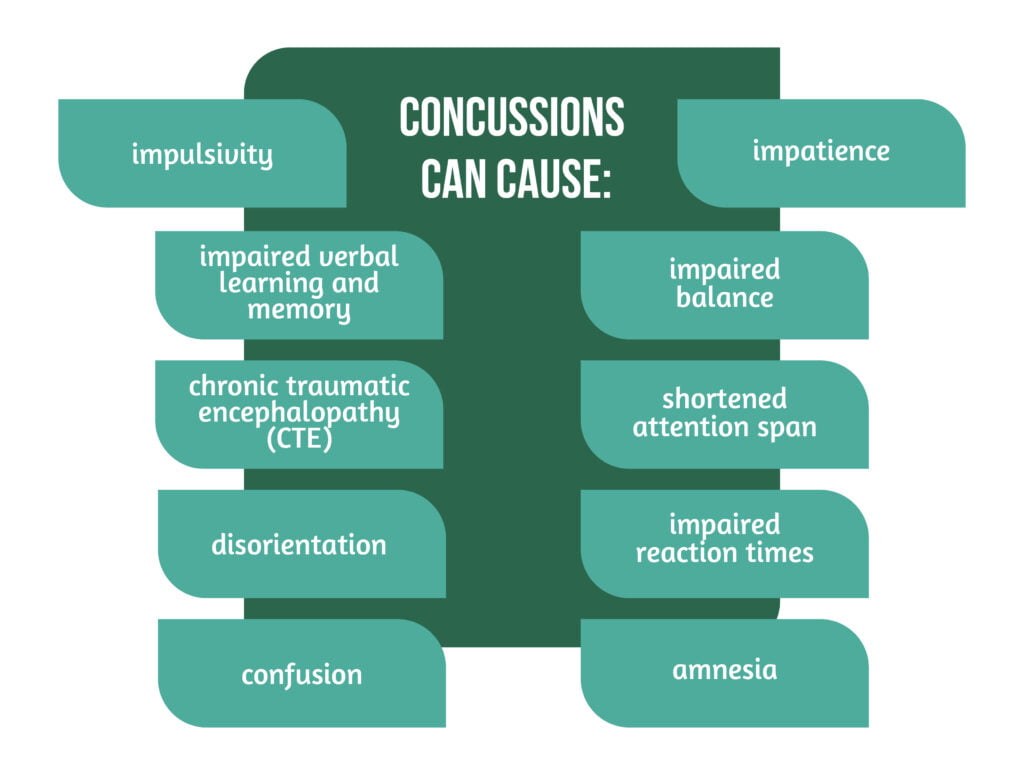
Sports-related concussions in children are a growing worry due to possible long-term effects on developing brains. However, likely, the annual number of concussions among US children under 18 years old is understated and ranges from 1.1 to 1.9 million. Concussions can harm one’s physical, mental, emotional, and sleep health.
Concussions can also cause several symptoms (Figure 1) [3–5].
Although the acute concussion signs and symptoms usually disappear in 7 to 10 days for adults, children frequently take longer to recover. Research shows that pediatric sports-related concussion recovery times range from 13 to 64 days. Age, sex, the number of prior concussions, and injury features such as symptom intensity, cluster, and burden are all linked to prolonged recovery in patients. Therefore, it will be easier to provide more effective care if researchers understand the healing patterns and length of juvenile sports-related concussions in the context of individual differences, acute injury features, and symptom burden [3].
While in older children and female sex, the number of prior concussions, subacute and acute symptoms, and symptom burden are prognosticators for extended recovery, recovery progression is still poorly understood. Therefore, for efficient management decisions and prevention methods, it is crucial to investigate the ordinary course of rehabilitation from concussion by age and sex. This is because sex differences persist throughout development and extensive brain growth, and significant cognitive development occurs throughout childhood [4].
Pathophysiology of SRC
The forces of head rotation, acceleration, and deceleration make up the biokinetics that cause SRC. According to current theories, biomechanical pressures to the head cause axonal deformation and rapid cellular alterations, such as ionic flow and glutamate release, which result in a metabolic imbalance between increased glucose requirements and reduced cerebral blood flow. This biochemical mismatch phase creates a window susceptible to re-injury [6].
Children are more likely to have weaker neck muscles, which could reduce the head’s ability to absorb impact and raise the risk of concussion. SRCs’ neurologic symptoms and signs are thought to represent functional or microstructural injuries rather than macroscopic neuronal damage. Findings imply that the developing brain may be more susceptible to axonal damage because myelination is a continuous maturational process throughout brain development. Despite the possibility of cell death resulting from all the post-injury alterations, there may not seem to be much of it following a concussion. At the moment, it is unclear how enduring anatomical alterations and cognitive impairment might develop [5].
Epidemiology
A recent study by Halstead and al. found that 75% of 5-17-year-old kids with sport-related concussions reached the healthcare system via their primary care practitioner. However, many epidemiologic research studies are based on emergency room visits. Some individuals might never seek medical attention for their injuries, which makes it more challenging to determine the true epidemiology. According to a pediatric study, 45% to 65% of concussion patients did not receive care in a medical setting. Underreporting by athletes who have SRCs is still a significant concern, particularly given that SRCs are typically not apparent injuries to an observer, necessitating self-reporting for identification [5].
According to other research, 66% of high school players who sustain concussions while participating in sports continue to compete for a range of reasons, including a lack of understanding by coaches, athletes, and parents, a desire to remain in the game, and a fear of addressing their coach [5].
Signs and symptoms of SRC
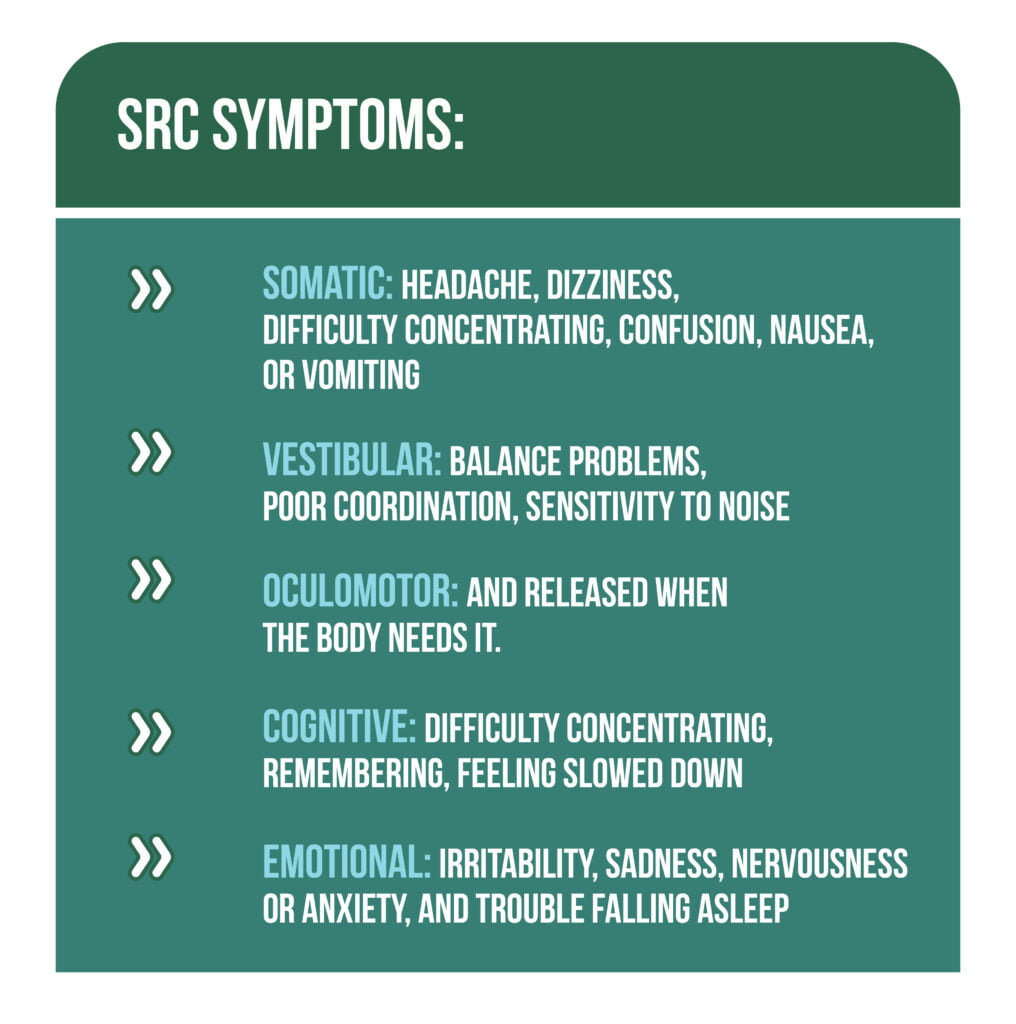
SRC symptoms can be divided into five groups: somatic, vestibular, oculomotor, cognitive, emotional, and sleep-related (Figure 2) [5].
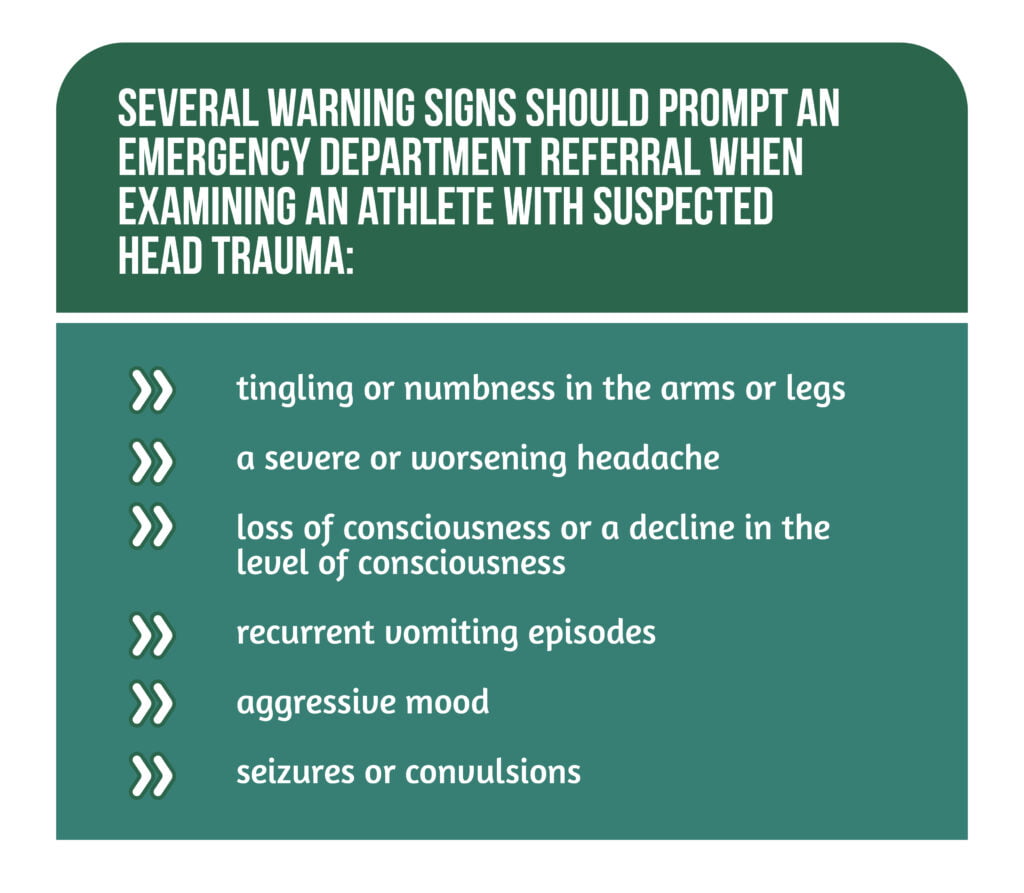
Repeated evaluations are necessary for athletes following head trauma since they may not always exhibit symptoms or abnormalities on their cognitive or balance tests right away. Several warning signs should prompt an emergency department referral when examining an athlete with suspected head trauma (Figure 3) [5].
Management of concussion
Athletes who are thought to have had a concussion need to be taken out of the game and not permitted to play again that day. According to numerous studies, young and college athletes who sustained concussions but continued to play displayed more symptoms and required more time to recover than those taken out of the game right away [5, 6].
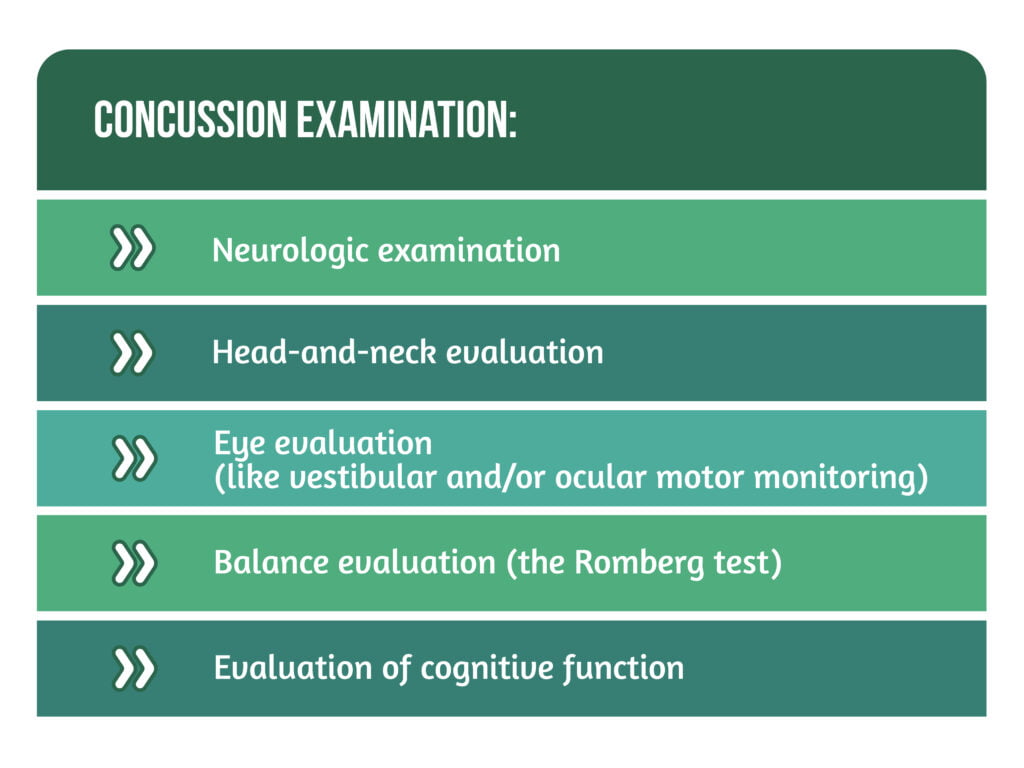
A physical examination may involve several steps (Figure 4).
In the immediate initial examination of concussion by coaches, sports trainers, or parents on the sidelines, sideline assessment tools, including the widely utilized Sports Concussion Assessment Tool (SCAT-5), created at the fifth International Consensus Conference on Concussion in Sport, are helpful. In addition, the SCAT-515 tool integrates five phases that address various concussion-affected domains into a side tool. However, it has yet to be approved as a return-to-play tool and should not take the place of a comprehensive physical exam by a doctor [5, 6].
The outcomes of standard neuroimaging are usually normal in concussion. Except in cases where there is a suspicion of a more serious intracranial damage or structural lesion (such as a skull fracture or hemorrhage), brain imaging tests like computed tomography (CT) or magnetic resonance imaging (MRI) of the brain do little to help with concussion evaluation and management. A substantial cervical spine injury, a skull fracture, or any of the four types of intracranial hemorrhage (subdural, epidural, intracerebral, or subarachnoid) may be linked to concussion.
Severe headaches, seizures, focal neurologic deficits, losing consciousness for longer than 30 seconds, significant mental status impairment, repetitive emesis, significant nervousness, and worsening symptoms are among the signs and symptoms that raise the index of suspicion for a more serious intracranial injury. A chronic subdural hemorrhage may not be completely ruled out by normal neuroimaging during the acute phase of injury, nor does it aid in predicting eventual neurobehavioral impairment or recovery time. Neuroimaging shows potential for imaging biomarker usage. However, more research and evaluation of these imaging techniques are still required, especially in children and adolescents [5, 6].
Cognitive and physical rest is the conventional advice for treating acute concussions. However, in a study conducted by Podolak, the authors highlight that for most children and adolescents, a few days of rest following a concussion, allowing the symptom burden to diminish, are sufficient, accompanied by a progressive return to physical and cognitive activity [6].
Adolescents with neurological, cognitive, learning, or psychiatric issues can benefit from the assessment, diagnosis, support, and rehabilitation skills that pediatric neuropsychologists are trained to provide. Cognitive tests and psychological assessments are also included in neuropsychological exams. A thorough clinical interview is frequently conducted, after which questionnaires, paper-and-pencil or computed cognitive function tests and validity testing are performed [6].
Return to school after concussion (RTS)
Children may have to stay home for several days after a concussion, with limited physical and mental activity to diminish acute symptoms. The ideal amount of time away from school has yet to be established and will likely vary depending on the symptoms’ type, severity, and persistence. To create a plan that works for the child in the context of their specific school environment and needs, the clinician monitoring the child’s care should collaborate closely with school employees. Students recover from concussions in various settings, including their homes, schools, future jobs, and social and sporting activities [6, 7].
A gradual return to the cognitive effort should be the aim of returning to school. The young athlete may attend all required classes as much as possible, gradually lengthening their time at school and eventually taking on a full academic load. To ensure a successful RTS for each concussed student, efficient communication between the school staff, medical team, the student, and parents/caregivers is crucial [6, 7].
Return to play after concussion (RTP)
Return to play for young athletes must be a highly personalized procedure because of the wide range of conditions they can experience. The Fifth International Conference on Concussion in Sport has established rules for RTP. The physician should determine if the athlete is prepared to resume play based on the athlete’s capacity for activity and specific observations from the detailed clinical examination. The higher risk of a second concussion or musculoskeletal problems should restrict athletes from returning to sports if persistent deficiencies in the oculomotor and vestibular evaluation or gait examination are found.
Studies have shown that children recover more slowly than collegiate athletes; therefore, a cautious approach should be used when deciding whether to return to play and whether a younger athlete is ready to resume their sport [6].
Athletes should not be permitted to resume contact, collision, or other high-risk activities until their concussion symptoms have subsided and they have finished the return-to-sport process. Athletes who have experienced many concussions in the past or who took a long time to recover (over 4 weeks) may require more time to complete each level of the process. Hiring an expert with concussion management knowledge may be necessary to develop a suitable return-to-activity plan [5].
Prevention
Given the heterogeneity in presentation, prevention, management, and rehabilitation, pediatric concussion is challenging and necessitates a multidisciplinary approach to provide children with the best care. Historically, attempts to avoid concussions have been concentrated on protective gear, education, rule adjustments, monitoring for elevated risk, and nutritional supplements:
- Protective gear: mouthguards, helmets, headgear
- Education: school employees, health workers, parents
- Monitoring for elevated risk: S100, glial fibrillary acidic protein, neuron-specific, enolase, and others are distinct biomarkers that have been researched for their potential to be used in concussion evaluation, but none of these are used in the clinical setting
- Supplements: numerous dietary supplements have been looked into for their potential to play either therapeutic or preventive roles in the management of concussions, yet there is presently no proof that these substances can improve the treatment or prevention of head injuries in people [5, 6].
Conclusions
Pediatric sports-related concussion diagnosis and treatment are continually improving as research progresses, leading to a greater comprehension of concussion’s neurophysiological and neurobiological bases and better patient outcomes. Pediatric and adolescent concussion therapy is distinct and complex, necessitating a strategy considering various variables. Initial evaluations should focus on the basic concussion domains of somatic, oculomotor, vestibular, cognitive, mood, and sleep. A thorough assessment and suitable, specialized rehabilitation of deficiencies in these areas are essential to effective treatment [6].
There is a wide range of intensity and types of symptoms for each concussion. These signs could be confused with those of other illnesses. Moreover, conclusive evidence regarding the long-term impact of a single concussion or numerous concussions is still lacking. Despite being significantly less common in younger athletes, repeated head trauma over a lengthy period has been linked to pathologic alterations in the brain in professional and collegiate players, as Halstead et al. showcased in their research. The precise relationship between pathologic findings and clinical symptoms is still being determined [5].
Pediatric student athletes’ return to everyday activities, academics, and potentially dangerous contact or impact sports is the aim of concussion management, which adds another level of complexity to care. Establishing objective indicators of recovery and considering the treatment received during recovery are essential areas for future research [3, 6].
References
- Brilliant AN, Meehan WP, Howell DR. Static and Dynamic Cognitive Performance in Youth and Collegiate Athletes With Concussion. Clinical journal of sports medicine: official journal of the Canadian Academy of Sports Medicine 2021. 31(5), 442–447. https://doi.org/10.1097/JSM.0000000000000779
- Howell DR, Myer GD, Brilliant A, Barber Foss K., Meehan WP. Quantitative Multimodal Assessment of Concussion Recovery in Youth Athletes. Clinical journal of sports medicine: official journal of the Canadian Academy of Sports Medicine. 2021. 31(2), 133–138. https://doi.org/10.1097/JSM.0000000000000722
- Thomas DJ, Coxe K, Li H, Pommering TL et al. Length of Recovery From Sports-Related Concussions in Pediatric Patients Treated at Concussion Clinics. Clinical journal of sports medicine: official journal of the Canadian Academy of Sports Medicine. 2018. 28(1), 56–63. https://doi.org/10.1097/JSM.0000000000000413
- Ledoux AA, Tang K, Yeates KO, Pusic MV et al. Natural Progression of Symptom Change and Recovery From Concussion in a Pediatric Population. JAMA pediatrics. 2019. 173. https://doi.org/10.1001/jamapediatrics.2018.3820
- Halstead ME, Walter KD, Moffatt K. COUNCIL ON SPORTS MEDICINE AND FITNESS. Sport-Related Concussion in Children and Adolescents. Pediatrics. 2018. 142(6), e20183074. https://doi.org/10.1542/peds.2018-3074
- Podolak OE, Arbogast KB, Master CL, Sleet D, Grady MF. Pediatric Sports-Related Concussion: An Approach to Care. American journal of lifestyle medicine. 2021. 16(4), 469–484. https://doi.org/10.1177/1559827620984995
- Purcell LK, Davis GA, Gioia GA. What factors must be considered in ‘return to school’ following concussion, and what strategies or accommodations should be followed? A systematic review. British journal of sports medicine. 2019. 53(4), 250. https://doi.org/10.1136/bjsports-2017-097853