Keywords: TBI, TBI outcome; TBI management; TBI prehospital management; emergency medical services; air ambulances; TBI epidemiology, emergency care
Prehospital care for severe TBI | what are the consequences?
Traumatic brain injury (TBI) is a heterogenic and complex pathology, considering the vast array of causes, mechanisms, clinical picture, management, and post-injury outcomes. All this makes TBI a burden to society due to the high mortality and morbidity leading to the need for treatment, rehabilitation, and care, as well as loss of productivity, associated financial costs, and impact on the patient’s environment. For society and patients, especially those severely injured, addressing and reducing post-TBI mortality and morbidity is of utter importance [1]. The consequences begin after the traumatic episode and can continue for years afterward.
Therefore, when addressing TBI to limit the extension of injuries, prevent further injuries and consequently improve the outcome of patients, it is critical to begin the management right after the injury, in the prehospital phase. Sebastiaan M. Bossers et al. studied the prehospital data regarding severely injured brain trauma patients (epidemiology, prehospital care, outcomes), intending to diminish the existing informational gap, thus increasing the knowledge for improvements of prehospital care [1–3].
The primary and secondary injuries of TBI
The diagnosis of TBI is frequently not difficult to establish, considering that the primary injury occurs at the moment of the traumatic episode. Still, the difficulty stands in the heterogeneity of causes, mechanisms, particularities of the affected person, and the prevention of secondary injuries leading to complications.
When considering TBI as a disorder, it is essential to note that the secondary injuries follow the primary injuries, thus the main targets of the TBI treatment and management include limiting of the extension of the primary injury and determining the factors involved leading to complications and further secondary injuries. The causes of primary and secondary injuries are showcased in Figure 1.
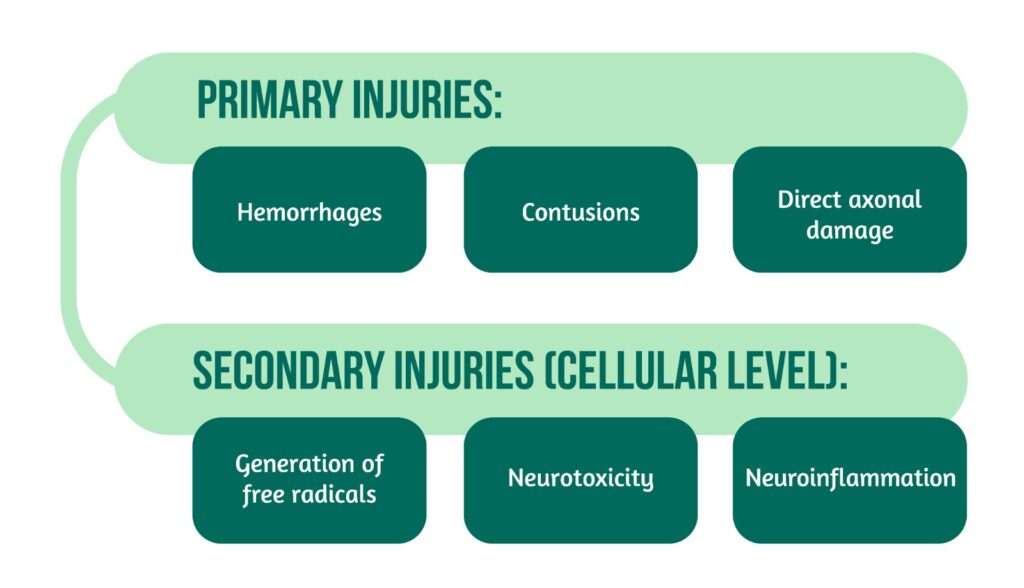
The secondary injuries appear minutes after the primary injury and can continue for long periods, leading, for example, to chronic traumatic encephalopathy years after the traumatic episode [1–3].
The management of TBI
Considering the patient’s injuries, a fundamental pillar in the management of TBI occurs in the immediate period, namely the prehospital phase, significantly impacting the patient’s outcome. The prehospital phase is usually followed by the hospital phase, which can include several departments depending on the severity of injuries:
- emergency department
- intensive care unit
- neurology department
- neurosurgery department.
During the prehospital phase, the management of TBI patients is focused on limiting the existing injuries and preventing the onset of new ones (secondary injuries), while addressing risk factors. This step is crucial as the secondary injuries can appear minutes after the primary affections, thus during the prehospital phase. Prehospital management refers to stabilizing the patient and ensuring proper oxygenation, blood pressure, and ventilation. However, a challenging problem is that most research on patients with severe TBI addresses the treatment received during the hospital stay and the subsequent recovery, while prehospital care still needs further research. Therefore, the guidelines approaching the prehospital healthcare of patients with severe TBI ought to be more precise and evidence-based to ensure the best outcomes [1–4].
Addressing the information gaps regarding prehospital treatment in patients with severe TBI
To overcome this problem, Sebastiaan M. Bossers et al. initiated a prospective, multicenter research in the Netherlands, namely the BRAIN-PROTECT study, covering the epidemiology, patient and operational characteristics, outcomes of patients and the mechanisms of trauma in patients with severe TBI during the prehospital phase. After extensive research on primary prevention, prehospital care, and treatment strategies, the study concentrated on patients for whom Helicopter Emergency Medical Services (HEMS) were used. Four HEMS exist in the Netherlands (Amsterdam, Groningen, Rotterdam, and Nijmegen) that can respond either with a helicopter or a modified ambulance (if needed or due to technical inability to use the helicopter) together with the assistance of a physician. These are used in cases of suspected major trauma, along with two regular ambulances.
In this study, the data collected from HEMS over 5 years within 9 trauma centers covered patients with a clinical suspicion of severe TBI based on the mechanism or clinical presentation combined with a Glasgow Coma Scale (GCS)<=8. Follow-up data were collected over an additional year after TBI. In addition, the centers covered information on in-hospital healthcare and patient outcomes, including Glasgow Outcome Scale (GOS) when discharged from the hospital and Glasgow Outcome Scale – Extended (GOSE) at one-year post-injury [1].
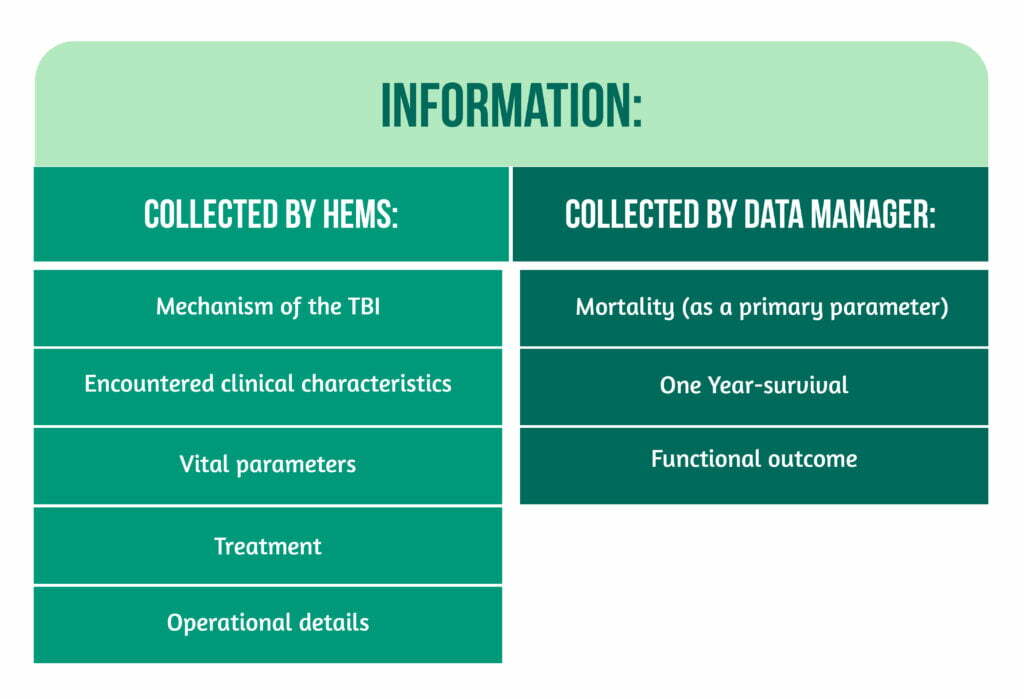
Information of variables was collected using pro forma reports, as showcased in Figure 2.
The study population was further stratified to ensure subgroup data analysis:
- “Confirmed TBI” for patients with a Head Abbreviated Injury Score (H-AIS) >=3
- “Isolated TBI” for patients with an H-AIS>=3 with the other elements of the scale<=2 [1].
Study results
Between 2012 and 2017, data was collected from over 2500 patients, 80% of whom attended a trauma center. The incidence rate of patients with suspected TBI (3.2/100.000 people annually) was close to the confirmed ones (2.7 /100.000 people annually).
Furthermore, the median age of patients was 46 years, varying between 1-97. A bimodal peak was identified, namely the first, during adolescence for females and young adulthood for males, and the second between 50-80 years of age. Most patients were males. Over 60% of the study population was healthy, with the remaining having comorbidities, mainly heart disease and increased blood pressure. Additionally, 14.2% of patients used anticoagulation (antiplatelet drugs, vitamin K antagonists, and low-molecular-weight heparin).
Although in 76.9% of the cases, HEMS attended the incidents, only 12.9% of these patients were transported by helicopter to the trauma centers. It is essential to mention that regarding the operational aspects, the median times were the following: from the sendoff to the injury scene – 18 minutes, on the injury scene – 16.5 minutes, transport to the hospital – 18 minutes with an overall time of intervention of 54 minutes. Two essential aspects must be mentioned. First, part of the HEMS was dispatched secondarily by ambulance to the scene. Still, a sensitivity analysis where HEMS and a vehicle ambulance were dispatched together showed identical median times. Moreover, the median distances for air and road travel differed from about 8 km (22.3 for air and 30.2 for road travel).
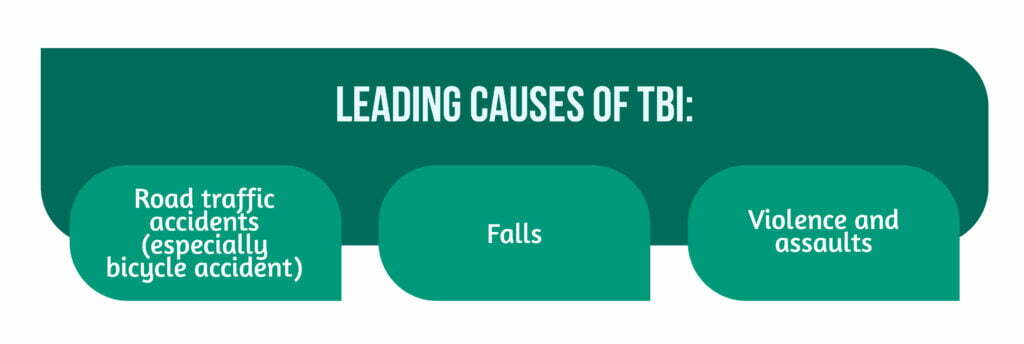
The three leading causes of TBI in the studied population were road traffic accidents, with a significant part being represented by bicycle accidents, followed by falls and, in a much more reduced manner, violence and assaults (Figure 3). Overall, most injuries were blunt, accidental, and on the road.
The clinical approach to establishing the severity of injuries used several scales, including the GCS. In this study, most patients had an initial GCS score of 3, with 13 patients, although initially having a score exceeding 8, consequently deteriorated to a lower score. The rest of the patients had GCS scores between 4 and 8. Moreover, the ISS was calculated in 1853 patients that were taken to trauma centers, with over 80% having a confirmed TBI and half of these patients having an isolated TBI. A median ISS score of 26 and an H-AIS score of 4 were determined. In addition to the clinical severity scores, computer tomography imagery scores were used (Rotterdam and Marshall).
The outcomes of patients covered the 30-day mortality, which increased proportionally with age and injury severity (mirrored in the GCS score and ISS score), leading to an overall death rate at 30 days of 39% and an overall one-year post-TBI of 42.1% in the studied population. It is noteworthy that most of the deaths occurred during the first 10 days after TBI. Regarding functional recovery, most patients had severe disabilities, although more than half presented a satisfactory recovery one year after TBI (as assessed with GOS-E) [1].
Considerations and particularities of the study
The incidence rate of severe TBI in other Dutch and European studies showed similar results, although two older studies from France and Norway showed higher incidence rates. The authors considered this contrast to be explained by differences between countries, a general decrease in TBI due to better primary prevention, or the use of different research protocols and definitions. Similarly, the median age and gender majority are consistent with previous studies, highlighting the youthfulness of the majority affected population and, consequently, the societal and economic impact due to healthcare costs and loss of productivity.
Furthermore, the bimodal age distribution contrasted with previous studies that showed a trimodal age distribution due to an identified peak in early childhood, contrasting the lack of severe TBI in young children in the Netherlands. The identified gender difference regarding the early age peak also offered information for shaping group-targeted primary prevention strategies.
Moreover, despite the healthy majority of patients, 80% over 65 had comorbidities (mainly cardio-vascular), and 50% were using anticoagulant drugs, possibly influencing the patient’s outcomes by aggravating their state. Similar to previous research, the leading causes were road traffic accidents and falls. Particularities of the study were emphasized by the fact that most crashes involved bicycle riding, reflecting their use on a large scale in the Netherlands compared to other countries, together with a lack of use of protective helmets. Falls happen in half of the elderly population at work or at home. Consequently, according to the authors, the prevention strategies should concentrate on these leading causes of TBI. Other particularities are the distances between trauma centers and the population density, mirroring the country’s increased development.
Moreover, this is also mirrored in the mean road distance, reduced use of the helicopter for transportation, and reduced time for HEMS interventions. Significant results regarding the patient’s outcomes included the mortality period for most patients within 10 days after TBI, which might have a future predictive value, and the 30-day mortality. Lastly, the mortality rates were lower compared to an older, similar Dutch study emphasizing either the differences between used protocols and definitions or the decrease in mortality during the period between the studies [1].
Conclusion of the study
Limitations of the study of Bossers et al. refer to exclusively monitoring HEMS interventions, thus possibly losing cases treated by vehicle ambulances and the exclusion of patients deceased at the scene, leading to an underestimation of the overall incidence rate of severe TBI. Nonetheless, the rate of treatable severely injured patients was emphasized, similar to previous studies.
The main conclusion is that through the data regarding the prehospital epidemiology and characteristics of severe TBI as well as outcomes, the existing informational gap on the subject has been diminished, and significant progress was made in the identification of better treatment strategies, allocation of resources, and future TBI research. A pillar has been added to future BRAIN-PROTECT studies regarding this subject. Nevertheless, the prehospital management of TBI remains a critical aspect impacting patient outcomes. Thus, further research in this field is needed [1, 4–5].
For more information regarding TBI, visit:
- Predicting access to rehabilitation: the CENTER-TBI approach
- What happens with social skills post-TBI?
- How can TBI patients’ caregivers manage stress?
Bibliography
- Bossers SM, Boer C, Bloemers FW, et al. Epidemiology, Prehospital Characteristics and Outcomes of Severe Traumatic Brain Injury in The Netherlands: The BRAIN-PROTECT Study. Prehosp Emerg Care. 2021;25(5):644-655. doi:10.1080/10903127.2020.1824049
- Ropper AH, Samuels MA, Klein JP, editors. Adams & Victor’s Principles of Neurology, 10th ed. McGraw Hill; c: 2014; p.885-903
- Jassam YN, Izzy S, Whalen M, McGavern DB, El Khoury J. Neuroimmunology of Traumatic Brain Injury: Time for a Paradigm Shift. Neuron. 2017;95(6):1246-1265. doi:10.1016/j.neuron.2017.07.010
- Maas AI, Menon DK, Steyerberg EW, et al. Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI): a prospective longitudinal observational study. Neurosurgery. 2015;76(1):67-80. doi:10.1227/NEU.0000000000000575
- Bossers SM, Boer C, Greuters S, Bloemers FW et al. Dutch prospective observational study on prehospital treatment of severe traumatic brain injury: the BRAIN-PROTECT study protocol. Prehosp Emerg Care. 2019;23(6):820–27. doi:10.1080/10903127.2019.1587126.




