Keywords: TBI, seizures, epilepsy
Focus keyword: seizures
Introduction – what is TBI?
Traumatic brain injury (TBI) represents one of the most important pathologies all over the world. As one of the essential public health concerns nowadays, this “silent pandemic” has a significant contribution to disability worldwide [1], presenting a high prevalence in industrialized countries [2] and often leading to complex sequelae. So, what should you do when experiencing post-TBI seizures?
One of the well-known complications after a brain injury is represented by seizures. Studies show that 1 out of 10 people who need hospitalization after suffering a TBI will develop seizures as a result of the injury, usually in a few days or weeks. However, there are reported cases of post-TBI seizures appearing months or even years after the traumatic episode. Of these patients, 70% to 80% are responding well to the antiepileptic drugs (AED) and can lead relatively normal lives, returning to most activities conducted before the incident. In contrast, a small percentage of patients have difficulties in day-to-day and social life due to complications of motor and cognitive abilities [3].
Find out more about the other effects of TBI:
- Can TBI affect emotions and behavior?
- Can TBI affect balance?
- What are the types of headaches associated with TBI?
- TBI and sexual functioning – what is the correlation?
What are seizures?
An epileptic seizure is defined as a transient occurrence due to abnormal synchronous and excessive neuronal activity in the brain [4]. During an episode, symptoms of seizures can occur, as seen in Figure 1.
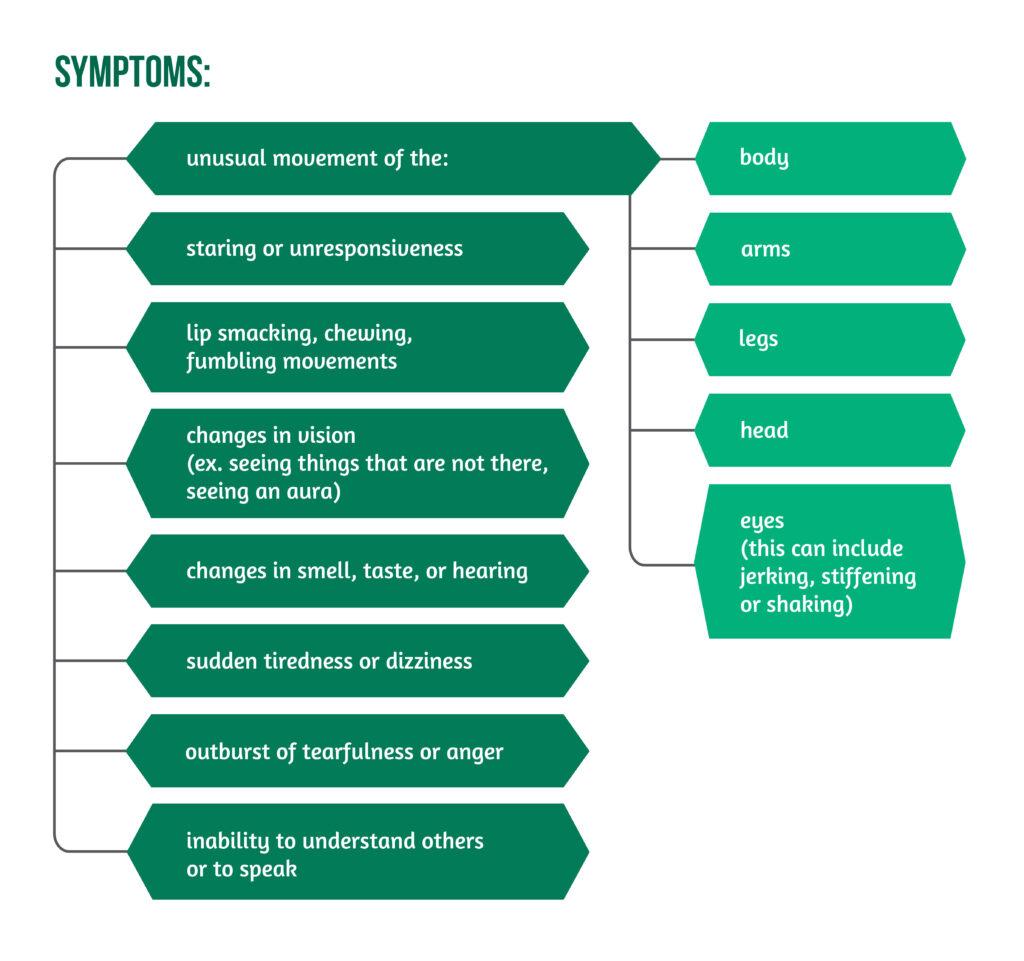
It is essential to understand that these symptoms appear suddenly and cannot be controlled by the patient. A seizure usually lasts a few seconds or minutes, manifesting with possible additional symptoms such as bladder or bowel accidents, as well as biting one’s tongue or the inside of the mouth. Patients might be weak, drowsy, or confused afterward, and symptoms can be even more severe after an extended episode [3]. Some conditions can increase the risk of seizures, as highlighted in Figure 2.

How do we know if the seizure is due to the TBI?
The first post-TBI seizures were described in the literature of Australian football players. They are considered to have different semiology from tonic-clonic seizures and can contain elements of primitive reflexes.
Research showed that one-half and one-third of the persons presenting in the Emergency Departments in England and Wales with a head injury are children. One-fifth of them have a skull fracture resulting from the TBI, and 15% of them need hospitalization as they might have had a seizure already, or the risk of one appearing is high [5].
Any seizure that occurs within the first week after the injury is called an early posttraumatic seizure. One that appears after this period is called a late posttraumatic seizure.
One quarter (1/4) of the patients with early posttraumatic seizures will repeat the episode after months or even years (leading to a diagnosis of epilepsy), in contrast to 80% of those with late posttraumatic seizures. In both groups, those who develop epilepsy usually respond to medication [3].
How can we treat seizures?
AEDs are drugs used to treat seizures, but they also influence mood instability, chronic pain, and restlessness. When deciding which AED to prescribe, doctors are thinking of both the well-being of the patient and the possible side effects presented in Figure 3 below.
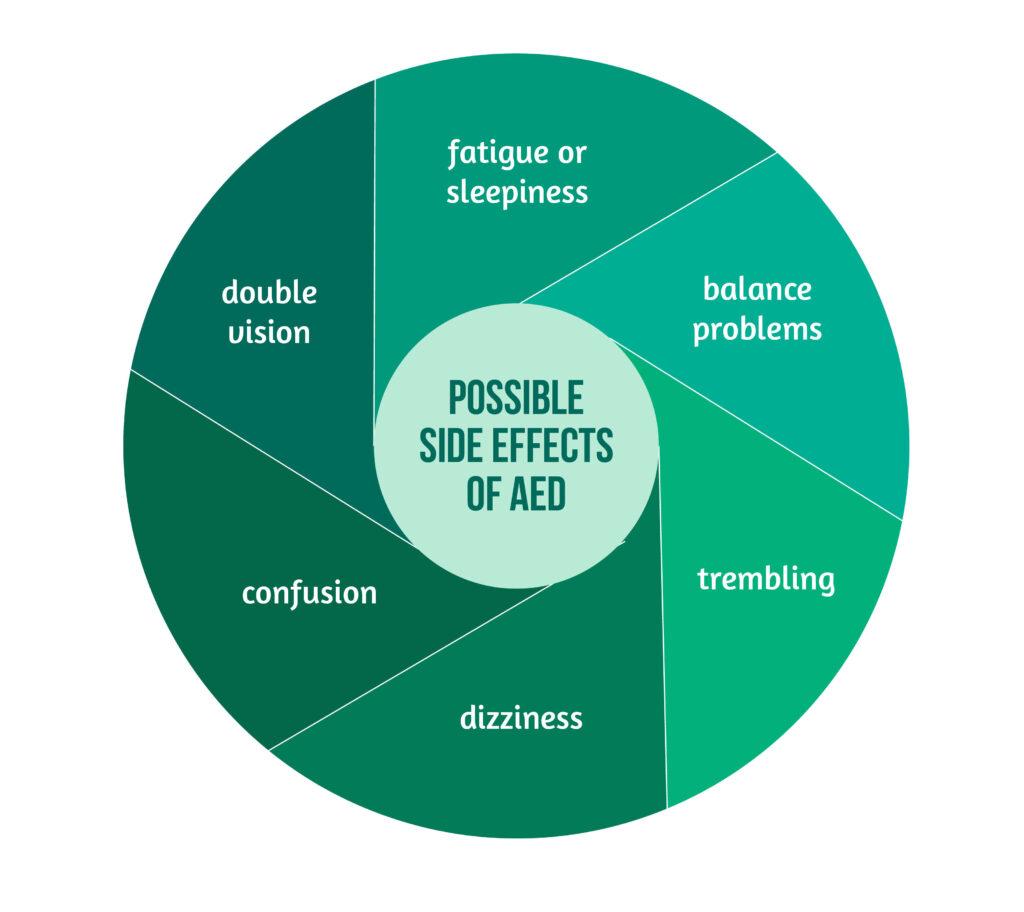
Female patients should always tell doctors if they are expecting or trying to become pregnant so the doctors can adapt the medication. If needed, doctors will prescribe two or more drugs to control the seizures.
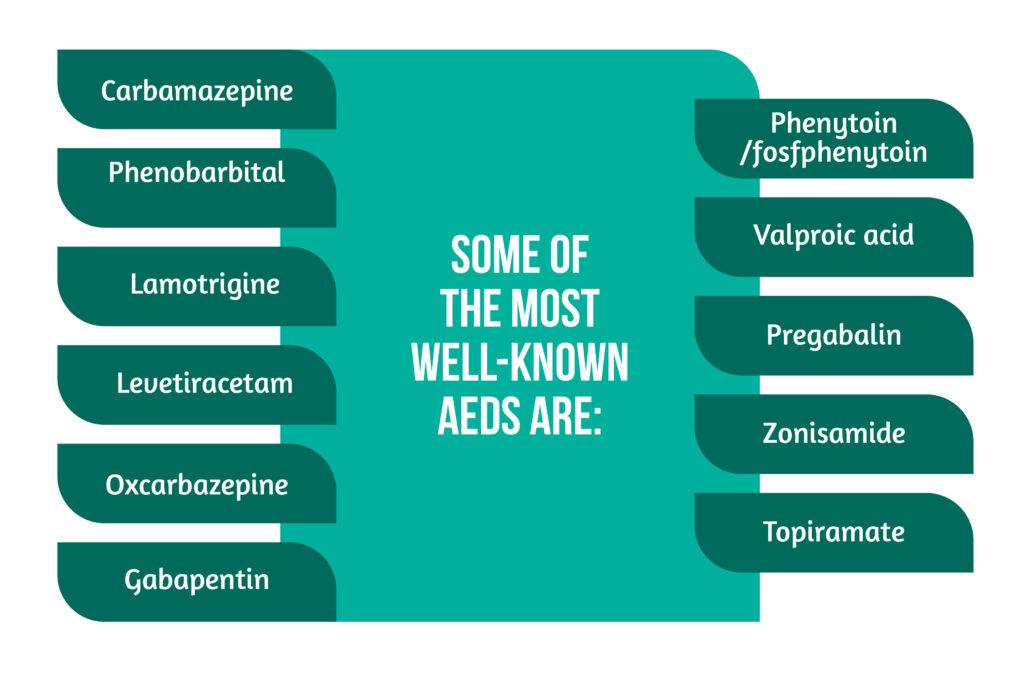
Some of the most well-known AEDs are presented in Figure 4 below.
Sometimes, anti-seizure medication cannot stop seizures. When this happens, patients are usually referred to an epilepsy center to be consulted by neurologists who specialize in epilepsy. Brain wave tests and video recordings of patients during a seizure are performed to find out the cause. The results help doctors decide the most appropriate course of medication.
What safety issues should patients know about?
In most countries, if a person has a seizure, they cannot drive for a certain period and must notify the department of motor vehicles.
The steps to take in order to stay safe in case of seizures are:
- talk to a specialist about the seizure risk based on the following:
- injury type
- the period since the injury
- medical status
- avoid drinking alcohol or using illegal drugs, as this might increase the risk of another seizure
- avoid operating heavy machinery after a seizure until discussing it with a doctor
- avoid climbing roofs, stairs, ladders, or tall objects
- always have someone close when being in the water (bathtubs, seas, lakes, oceans)
- when eating in restaurants, instruct friends on what to do in the case of a seizure or choking [3].
What should caregivers do in case of a seizure?
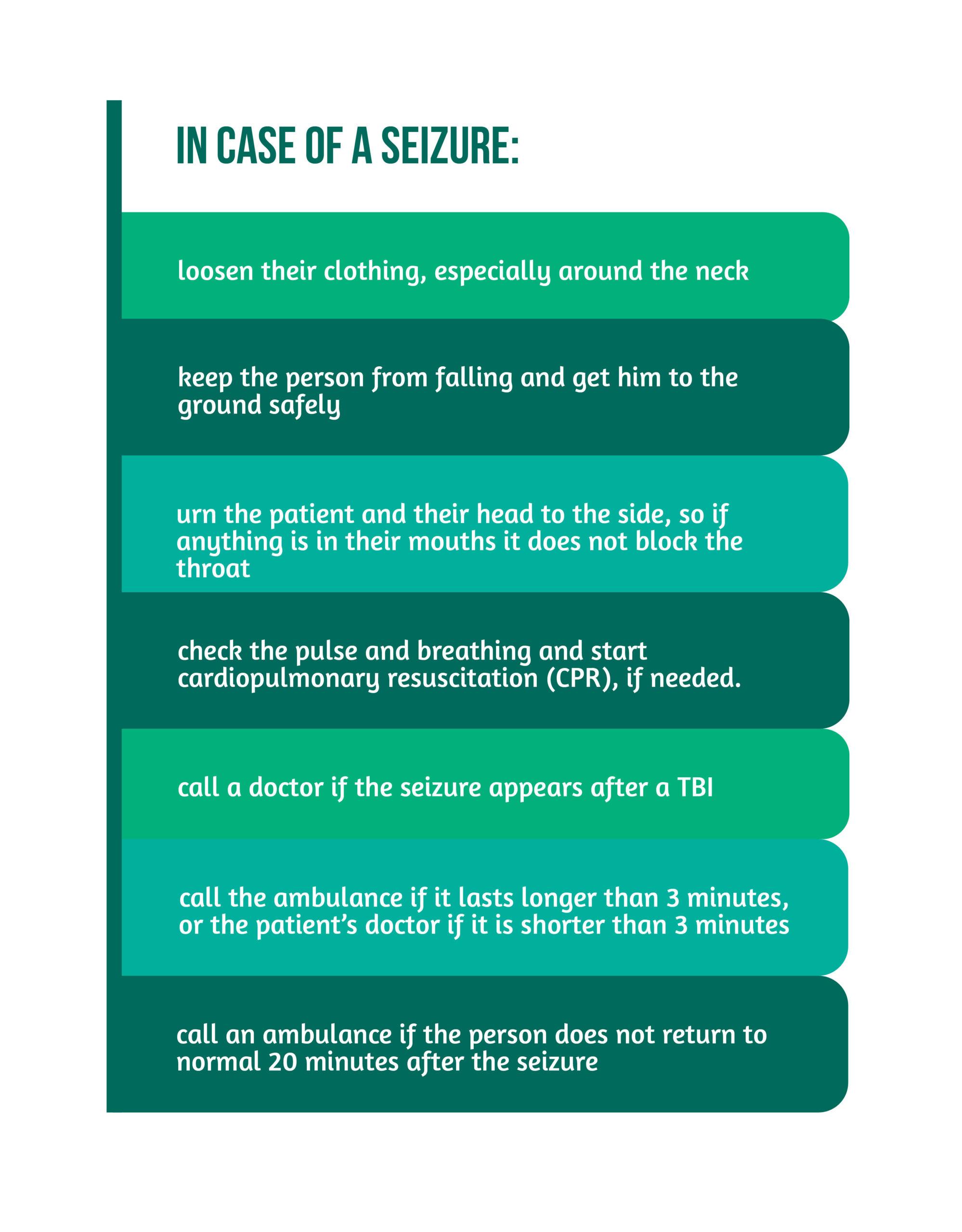
Family, friends, and caregivers should remain calm and watch the seizure in order to describe it later to the doctor. It is recommended to have a seizure diary where each event is written down with the date, time, duration, and a short description. Healthcare workers need to explain to the caregivers what to do to keep the patient from hurting himself in case of a seizure. The advice is presented in Figure 5 below.
What are the conclusions?
Seizures after a TBI represent common complications, especially of moderate to severe head injury, and they can appear even years after the event. Mechanisms of epileptogenesis are intensively studied nowadays in order to fully understand their mechanism of appearance and to improve, as much as possible, the treatment [5].
Post-TBI seizures represent a dire issue for the patients, their families, and doctors, and it is important to know how they present and how they can be treated so that the patient can lead a life as normal as possible.
References
- Dewan MC et al. ‘Estimating the global incidence of traumatic brain injury’, J. Neurosurg. 2018. doi: 10.3171/2017.10.JNS17352.
- Vakil E. ‘The effect of moderate to severe traumatic brain injury (TBI) on different aspects of memory: a selective review’, J. Clin. Exp. Neuropsychol. 2005. doi: 10.1080/13803390490919245.
- ‘Seizures After Traumatic Brain Injury | Model Systems Knowledge Translation Center (MSKTC)’. https://msktc.org/tbi/factsheets/seizures-after-traumatic-brain-injury
- Huff JS & Murr N. ‘Seizure’, in StatPearls, Treasure Island (FL): StatPearls Publishing, 2022. Accessed: Jun. 06, 2022. [Online]. Available at: http://www.ncbi.nlm.nih.gov/books/NBK430765/
- Fordington S & Manford M, ‘A review of seizures and epilepsy following traumatic brain injury’, J. Neurol. 2020. doi: 10.1007/s00415-020-09926-w.