Keywords: TBI, hypoxemia, respiratory, ARDS, ventilation
Introduction
VENTILatOry Strategies in TBI – are there new Avenues for Acute Respiratory Distress Syndrome (ARDS) patients? Traumatic brain injury (TBI) represents a serious health, social, and economic problem worldwide. The causes of TBI are showcased in Figure 1 below.
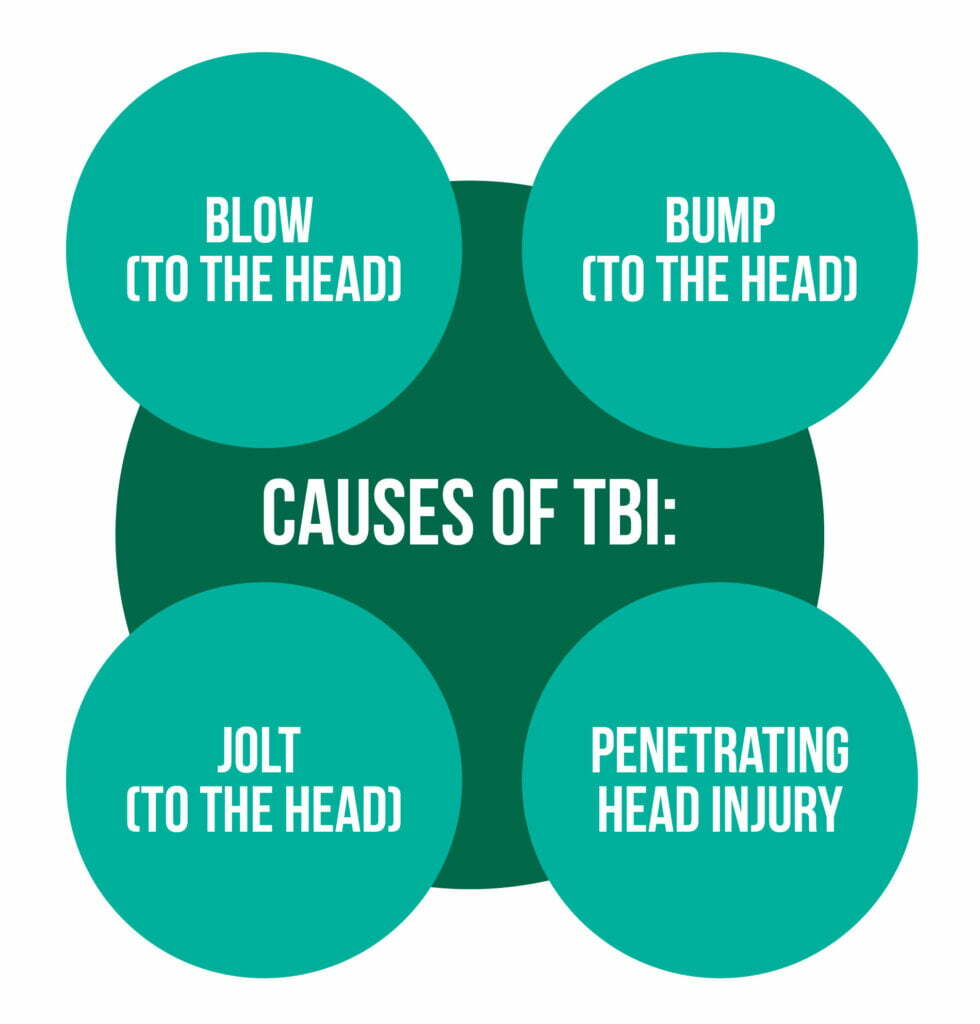
This has the consequence of disrupting the normal function of the brain, according to the US Centers for Disease Control and Prevention (CDC). However, not all jolts or blows to the head have the necessary force to cause a brain injury. The most common causes of TBI for active military personnel in war zones are blast exposures and the accompanying overpressure wave. A TBI severity can range from mild to severe [1–3].
Worldwide, the disability and mortality rates caused by TBI remain high. Severe TBI patients with altered consciousness frequently need intubation and invasive mechanical ventilation in order to protect the airways from aspiration and to prevent any secondary insults, such as hypoxemia and hypercapnia.
Hypoxemia = the lowering of the partial pressure of oxygen below 60 mm Hg
Hypercapnia = the rise in the partial pressure of CO2 above 45 mm Hg [4].
During long stays in the therapy units, patients may develop acute respiratory distress syndrome (ARDS) and secondary respiratory failure. Hyperventilation is used in most centers in the case of patients with severe TBI but only for short periods of time [5]. Current strategies focus on lung-protective ventilation with moderate-to-high positive expiratory pressure (PEEP) and low tidal volumes (TVs), strategies shown to improve outcomes for patients suffering from ARDS and non-ARDS. Moreover, PEEP and TVs are characterized by permissive hypercapnia and “low ranges” oxygenation targets, making them difficult to apply in TBI patients due to its potential cerebrovascular adverse effects, regardless of the presence of high intracranial pressure. Usually, in TBI patients, high TVs and low PEEP are applied for tight CO2 control, but recent studies showed that high TVs are associated with acute lung injury development. This is why brain-injured patients have been excluded from major trials that explored lung-protective ventilation strategies in ARDS [4].
The study by Picetti et al. from 2020 aimed to perform an international survey that investigated current practices in respiratory management in the cases of TBI patients with or without respiratory failure.
Methodology
The current survey was endorsed by the European Society of Intensive Care Medicine (ESICM) and promoted by Acute Respiratory Failure (ARF) and the Neuro-intensive Care (NIC) sections.
An electronic questionnaire that included 3 clinical scenarios and 38 items were available on the ESICM website for 5 months, from November 2018 until March 2019. The questionnaire was created by two scientists following a non-systematic review of the literature on the respiratory management of TBI patients. It was designed to identify:
- the participants’ demographics, available neuromonitoring tools, and type of hospital/specialty
- protocols for mechanical ventilation and weaning
- respiratory management strategies ESICM members that treated patients with TBIs in their clinical practice were the main target. They were also invited to involve more respondents from their local hospital [4].
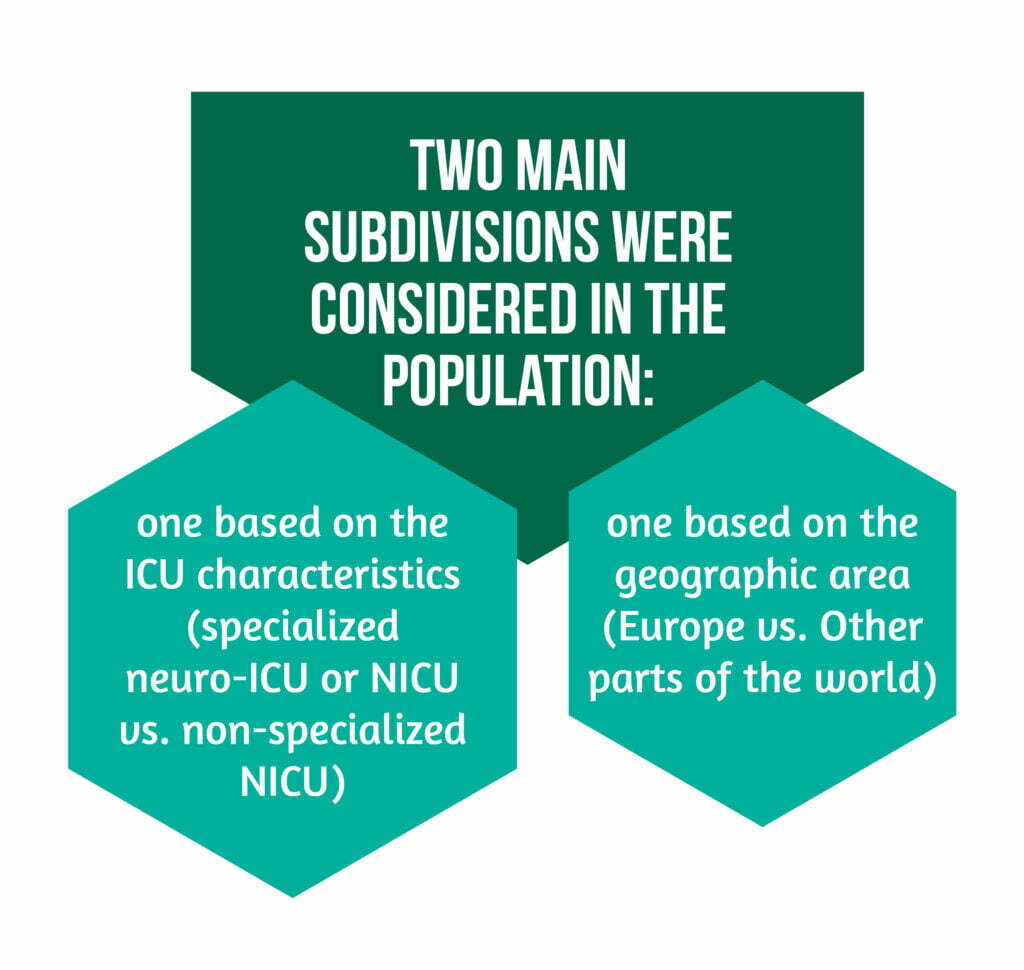
Two main subdivisions were considered in the population, as showcased in Figure 2.
Results of the research
From a total of 676 participating centers, there were a total of 687 respondents. Most respondents were located in Europe – Italy being the country with the highest number of participants-, followed by Sudan, the USA, and Brazil. The majority of respondents were intensivists and anesthesiologists working in mixed general and NICUs.
The results revealed that most participants used a standard protocol for mechanical ventilation in TBI patients along with a specific weaning protocol.
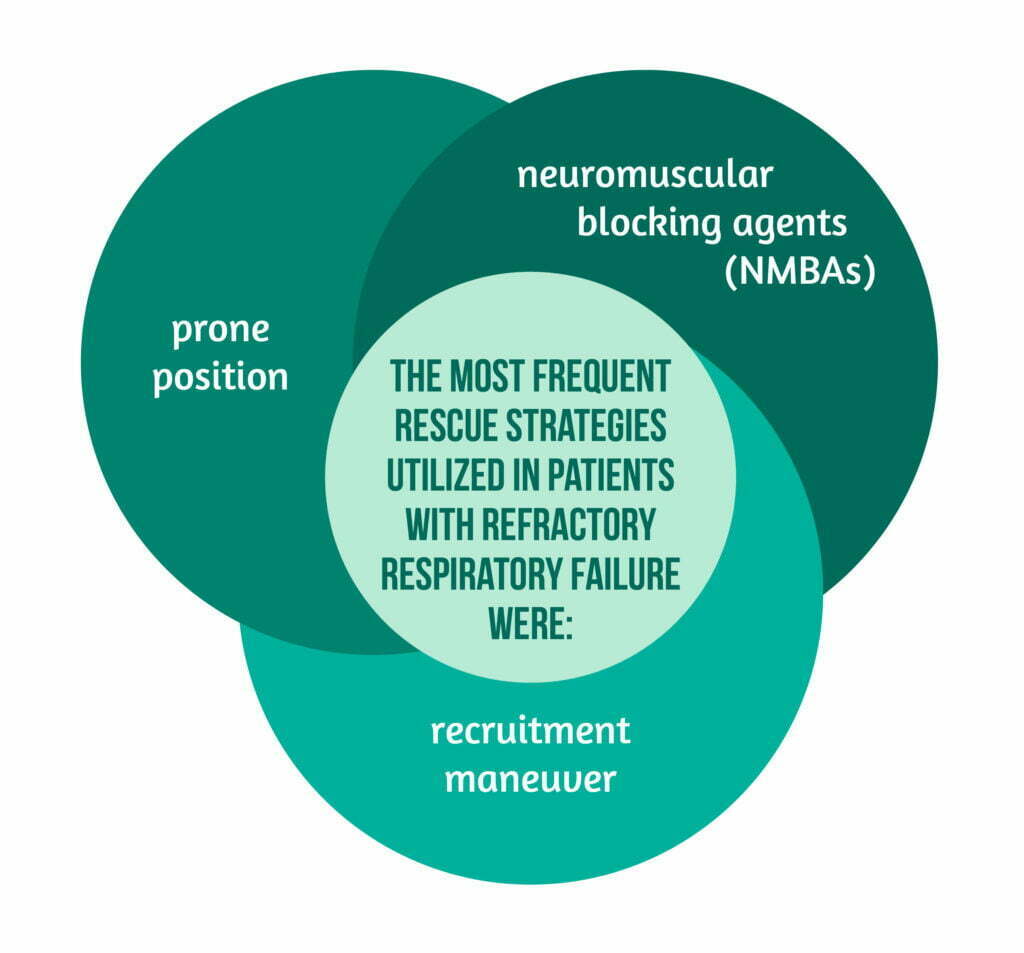
The most frequent rescue strategies utilized in patients with refractory respiratory failure are highlighted in Figure 3.
European respondents, compared to non-European ones, had higher PaO2 targets and less frequent use of plateau pressure targets of under 30 mmHg
In terms of neuromonitoring, specialized NICUs, compared to non-specialized NICUs, had more available monitoring tools.
Discussion
The study of Picetti et al. revealed one of the largest surveys published regarding ventilator strategies in TBI patients. With worldwide respondents, the results describe worldwide strategies used nowadays in the clinical practice in this field. The main results of this survey can be summarized as follows:
- a small number of respondents utilized specific mechanical ventilation protocols and weaning in TBI
- low TVs and a PaCO2 with a target of 36-40 mmHg are most frequently utilized
- in the case of intracranial hypertension, lower levels of PEEP are employed
- in the case of refractory respiratory failure, NMBAs are the most common rescue strategy
- great variability in practice exists [4].
The impact of TVs on the respondents
In patients with or without ARDS, lung-protective ventilation strategies were shown to have an impact on their outcome. Especially low TVs are an important component and are associated with reduced mortality in ARDS patients. Although research showed it could also cause hypercapnia and, as a result, cerebral vasodilatation, high TVs in TBI patients with normal lung function at admission is associated with the possibility of developing ARDS. Future research is necessary for TBI patients to establish optimal TV values. The majority of the survey respondents declared using low TVs in these patients, even in specialized NICUs [4].
PEEP is another important component of lung-protection ventilation, improving PaO2 and lung compliance, and reducing atelectasis. Due to its possible effect on cerebral circulation and intracranial pressure (ICP), low PEEP levels under 5 mm Hg have been used in TBI patients. High PEEP levels are linked to reduced systemic venous return and cerebral perfusion pressure (CPP) with consecutive consequences on cerebral blood flow (CBF) and mean arterial pressure. On the other hand, the effect of PEEP on brain circulation and ICP is influenced by respiratory system compliance. Patients with low compliance do not show an increase in the ICP if there is a PEEP increase up to 10-12 cmH2O. In contrast, patients with normal compliance show a reduced cerebral venous return and an increase in ICP due to the fact that PEEP induces lung overdistension. The fact that most of the survey respondents said that they use lower PEEP levels suggests that there is a general concern regarding the cerebrovascular effects on the ICP of PEEP. Moreover, physicians recognized they tend to use higher PEEP values in patients without intracranial hypertension, which contradicts the nowadays evidence challenging the utility of the “open lung approach”. Better neurological and cardiological monitoring tools are needed in order to identify the optimal PEEP value in head-injured patients [4].
Use of hyperventilation
Also, the survey data presented the fact that hyperventilation is not often used in TBI patients. This is probably due to the fact that there are potential ischemic adverse effects of hypercapnia on the injured brain. For now, hyperventilation is suggested only in case of emergency, when there is a life-threatening risk of cerebral herniation. Recent studies indicated that hyperventilation is able to reduce the ICP, but does not have a clinically significant impact on cerebral oxygenation and metabolism. Most responders aimed for a CO2 value of 36-40 mmHg, and only a minority of them accepted mild hypercapnia, even in the cases without intracranial hypertension.
Also, the majority chose a target level of PaO2 between 81-100 mmHg, higher than the ones used in ARDS patients, which is about 55-80 mmHg. Just a minority of respondents accepted mild hypoxemia, mostly in non-specialized NICUs. This decision can be linked to the concern of hypoxia and its adverse effects on brain-injured patients, but mostly, to the recent studies that showed the risks of hyperoxia on critically ill patients [4].
Rescue Maneuvers
Several rescue maneuvers can be applied in the case of refractory respiratory failure besides invasive mechanical ventilation to ameliorate gas exchange. NMBAs have been used in ARDS patients to improve gas exchange and mortality. The survey respondents recognized that neuromuscular blockade is the most frequently used strategy, probably due to its possible beneficial effect on intracranial hypertension. However, they present possible side effects (muscle weakness) and should only be reserved for severe cases [4].
There is a potential benefit on lung injury and gas exchanges of recruitment manoeuvers with the possibility of reducing atelectasis and increasing lung expiratory volumes. A recent study, however, questioned their use, showing increased mortality in ARDS patients who underwent lung recruitment manoeuvers and titrated PEEP vs. low PEEP. These manoeuvers can also have potential adverse effects on the injured brain, causing increased ICP, comparable to the application of high levels of PEEP. Even so, in the current survey, they were the second most used rescue strategy. In TBI patients, neuromonitoring seems to be mandatory in order to be able to improve systemic oxygenation without causing serious side effects [4].
Due to its ability to increase end-expiratory lung volume, improve ventilation/perfusion ratio, and decrease VILI by ameliorating the TV distribution prone position remains frequently used in patients suffering from ARDS. It is shown to reduce the mortality of these patients if it is applied for more than 12 h/day and in patients with a PaO2/FiO2 lower than 150. So far, a small number of studies have been published involving patients with neurological damage. Despite an improvement in the systemic/brain oxygenation, there was often observed an increase in the ICP. As a result, patients with TBI or other neurological damage have generally been excluded from the only prone position trial in ARDS patients [4].
Extracorporeal membrane oxygenation
In recent studies, for these patients, ECMO (extracorporeal membrane oxygenation) has been evaluated as a rescue strategy. Historically it was not utilized in TBI patients due to the fact that there is an associated risk of cerebral bleeding related to the use of anticoagulants, but recent studies showed a potential benefit of ECMO. Nearly half of the survey respondents agreed they would use ECMO as a respiratory strategy in TBI patients, as there could be the possibility of adopting heparin-free venovenous ECMO, which has lower risks of bleeding complications. Nevertheless, further investigations are needed regarding the use of ECMO in TBI patients.
A small number of respondents suggested the use of extracorporeal CO2 removal (e.g., DECAP), but a small dose of heparin is needed as it carries a risk of bleeding. This method is rarely used in clinical practice due to its limited efficacy [4].
Limitations and Conclusions
The current survey has several limitations. The response rate could not be calculated based on its design, and the fact that ESICM members were encouraged to bring more participants locally, makes it impossible to determine the total number of persons who received the survey. Also, respondents from specialized NICUs were included with those working in general ICUs. Moreover, the survey was developed by two investigators without a prior systematic review of the literature. Finally, it only refers to physicians’ clinical practice in the respiratory management of patients that suffered a TBI, and it does not include any of the patients’ data [4].
The study of Picetti et al. [4] shows that there are still differences in the clinical practice regarding ventilator management of TBI patients, with or without any existing respiratory failure. Lung-protective ventilation strategies seem to be more and more used by clinicians, even with the concern regarding high PEEP in patients with high intracranial pressure.
Further studies are needed in order to determine the best strategy for these patients and to clarify the existent variability between centers.
For more insight into other TBI-related topics, visit:
- Alcohol consumption and TBI: a continuing problem for patients and society?
- Quality Indicators for TBI Patients
- Prevention of Neurotrauma is the best treatment
Bibliography
- Faul M and Coronado V, ‘Epidemiology of traumatic brain injury’, Handb. Clin. Neurol., vol. 127, pp. 3–13, 2015, doi: 10.1016/B978-0-444-52892-6.00001-5.
- ‘Injuries from explosions: physics, biophysics, pathology, and required research focus – PubMed’. https://pubmed.ncbi.nlm.nih.gov/19430256/ (accessed Jul. 18, 2022).
- Majdan M, Plancikova D, Brazinova A, Rusnak M. ‘Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis’, Lancet Public Health 2016, vol. 1, no. 2, pp. e76–e83. doi: 10.1016/S2468-2667(16)30017-2.
- Picetti E et al., ‘VENTILatOry strategies in patients with severe traumatic brain injury: the VENTILO Survey of the European Society of Intensive Care Medicine (ESICM)’, Crit. Care Lond. Engl. 2020. doi: 10.1186/s13054-020-02875-w.
- Galgano M, Toshkezi G, Qiu X, Russell T, Chin C, and Zhao L-R. ‘Traumatic Brain Injury: Current Treatment Strategies and Future Endeavors’, Cell Transplant., vol. 26, no. 7, pp. 1118–1130, Jul. 2017, doi: 10.1177/0963689717714102.