Keywords: TBI, military, civilian, recovery, mTBI
Introduction | Military and civilian TBI
Traumatic brain injury (TBI) is a significant problem in civilian and military populations. TBI significantly impacts the individual through the persistence of cognitive disorders and the decrease in quality of life. Therefore, rapid diagnosis and appropriate treatment are necessary to avoid secondary injuries.
The research by Lamberty et al. highlighted the similarities and differences in the evaluation and treatment of both civilian and military TBI patients. Brain trauma assessment is carried out in the same way in both environments, as is the determination of the degree of disability [1].
Establishing the severity of TBI
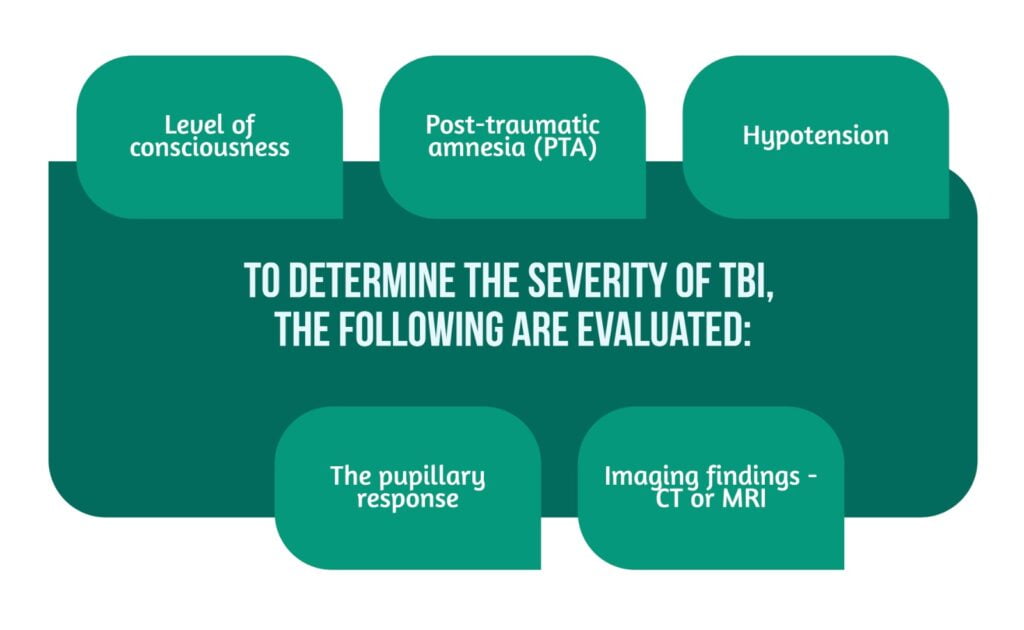
In the case of patients with TBI, the detailed evaluation of the lesions is essential to establish the prognosis. Determining the severity of traumatic brain injury is done by evaluating the following factors:
- Level of consciousness is evaluated using the Glasgow Coma Score (GCS) or other corresponding tools, but it cannot predict the evolution of the patient’s condition. Therefore, these scores are used to monitor patients but cannot determine the degree of damage or the prognosis after the TBI [1].
- Post-traumatic amnesia (PTA) is the best clinical predictor in establishing the recovery prognosis after TBI. After a TBI, patients can develop cognitive disorders, and with memory and attention impairment, they can become confused or agitated. There is no clear correlation between the GCS score and the duration of post-traumatic amnesia. In the case of many patients, the TBI can be classified as mild using the GCS score, but they present increased durations of PTA, suggesting a severe form of TBI [2].
- The pupillary response is an examination that can be performed even in the case of an unconscious patient and monitors pupillary asymmetries, the size, and the reactivity of the pupils to light. Identifying a pupillary abnormality leads the doctor to suspect increased intracranial pressure (ICP) due to increased cerebral edema or hematomas [3].
- Imaging findings – CT or MRI are the methods used in patients with TBI. Imaging examinations help to diagnose brain lesions, skull fractures, and hemorrhages. Moreover, the signs of intracranial hypertension (ICP) can also be detected. ICP is a significant complication of brain trauma that can lead to cerebral herniation with the compromise of vital functions and death [4].
- Hypotension is associated with poor outcomes in TBI patients. Thus, maintaining systolic blood pressure above 110 mmHg is recommended [5] (Figure 1).
Documentation of TBI in civilian versus military population
In the civilian population, any presentation to the hospital due to TBI is recorded, thus helping to establish treatment, subsequent follow-up, and litigation regarding injury and disability.
In the military population, accidents due to exposure to improvised explosives or other traumatic events are increasing. As a result, service members with life-threatening injuries are consistently treated at the scene of the accident. Military members are not always carefully monitored after a TBI, in many cases returning to work without benefiting from a recovery period to administer the treatment and ensure the healing of the wounds. Even in the civilian population, some minor injuries will not receive medical treatment due to the victim not presenting in a medical unit [1].
Rates of moderate/severe TBI
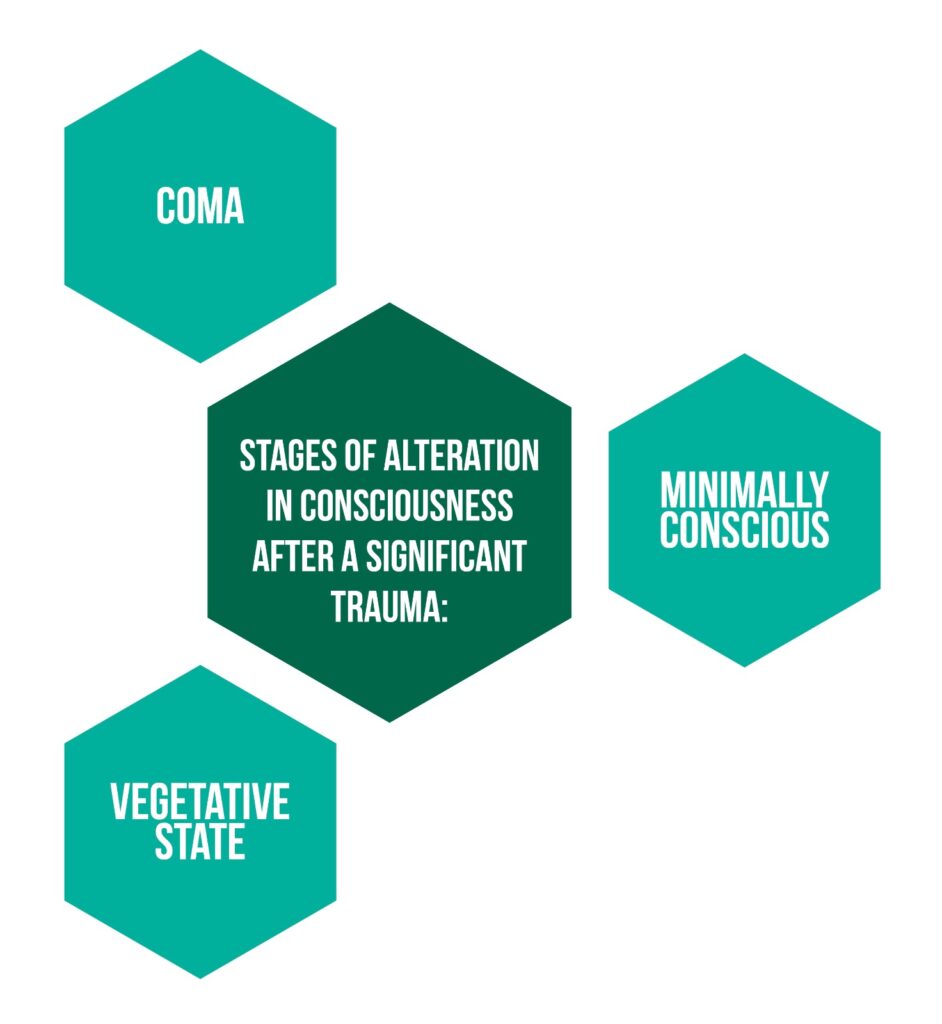
It is estimated that 10% of hospitalized patients with TBI have moderate forms, and another 10% have severe forms of TBI. The severity of TBI depends on the severity of the primary injury but also on the secondary factors (abscess, hypoxia, intracranial hypertension, hypotension) that can cause the patient’s condition to worsen. The alteration in consciousness after a significant trauma includes the following stages: coma, vegetative state, and minimally conscious (Figure 2). The evolution of each patient is different. Some stay for a long time in a particular stage, and others can quickly pass from one stage to another [1].
Approximately 40% of patients with severe TBI die, unlike moderate forms of TBI, where death occurs in only 10% of victims. Furthermore, after severe brain trauma, 1-3% of patients can be in a vegetative state, and 30% have a severe disability, unlike moderate TBI, where severe disability rarely occurs. Only 25% of the victims will have a moderate disability in the following months after the trauma [1].
TBI Screening
Identifying the cases of TBI is necessary, especially in patients with chronic symptoms, decreased cognitive performance, and poor integration into society. The effects of a TBI can appear with a delay, so the screening and documentation of any head trauma are important. For example, in children, the effects of TBI will not be seen immediately. They may develop normally, and the deficiencies may be evident only when the social and academic demands become more complex. Moreover, studies have shown that people with a history of TBI have an increased risk of re-injury. Patients who suffer repetitive head trauma have more severe consequences due to the cumulative effect of multiple injuries [6].
Screening for traumatic brain injury helps establish the actual incidence of TBI and the consequences on the individual and society, helping to develop preventive measures and standardize the treatment [6].
Returning to work after moderate or severe TBI
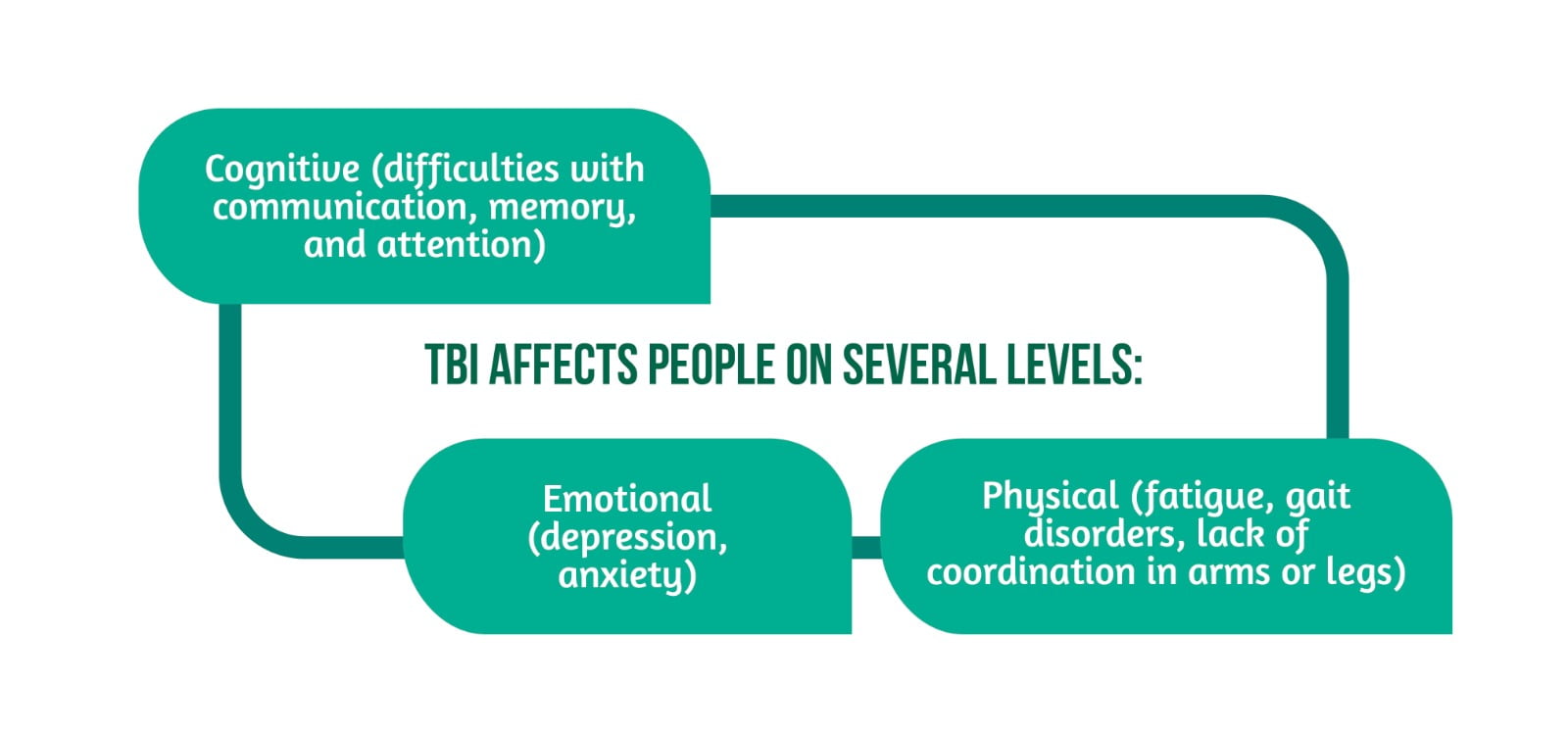
TBI leads to cognitive, emotional, and physical affections (Figure 3) that prevent individuals from returning to work shortly after the injury. A smaller number of patients with moderate and severe forms of TBI will return to work after trauma than those with mild TBI [1].
In a study by Dickmen, it was found that 38% of severe TBI patients and 66% of moderate TBI patients had returned to work two years post-cerebral trauma. The proportion of patients who can resume their daily activities and go to work is higher among patients with mild TBI [1].
Veterans with moderate and severe TBI
It is estimated that 266,000 veterans underwent TBI between 2000 and 2012, with only 9% having moderate and severe forms of TBI. Nowadays, survival rates after a TBI are higher due to improved medical care and progress in military armor development [1].
Special attention was also paid to the psychological component when considering soldiers with TBI. For this reason, the psychological status of military personnel at discharge was compared with the total population discharged. Studies have shown that patients with TBI are 1.8 times more prone to behavioral disorders without identifying a significant difference between patients with moderate and severe TBI and the total population discharged from the hospital. In addition, the number of outpatient visits is higher in the case of severe and moderate trauma, and veterans with TBI have a higher risk of neuropsychiatric conditions such as chronic pain and PTSD. Moreover, existing cognitive deficits determine a variable degree of disability [1].
Mild TBI
Most patients with cranial injuries from the civilian and military population suffer from mild forms of TBI. The actual incidence is unknown as victims of mild TBI do not present for medical care, considering the rapid resolution of symptoms. The main causes of TBI in the civilian population are falls, motor vehicle accidents, and being struck by or against a heavy object. Blast is the most common TBI cause in the military population. Therefore, brain trauma is the second cause determining the need for the neuropsychologist’s intervention in the patient’s recovery [1].
At the level of military personnel involved in the conflicts in Iraq and Afghanistan, the incidence rate of minor TBI varies between 9 and 22%, with the leading cause of brain trauma being blasts. Minor injuries remain a significant and costly problem both in the general population and in the military [1].
Rating the severity of TBI
The scheme established by the Department of Defense and Department of Veterans Affairs (DoD/DVA) can be used to determine the severity of a brain injury. Mild TBI is characterized by the lack of changes on brain imaging, a short period of less than half an hour of LOC, and a GCS with values between 13 and 15.
Determining the severity of TBI is based on acute symptoms and parameters. Knowing the acute elements helps the clinician evaluate if the patient’s recovery proceeds according to the severity of the trauma, but also to identify alternative factors (e.g., secondary gain, post-injury stressors) that determine the persistence of symptoms [1].
Recovery patterns and cognitive outcomes in TBI patients
Clinical neuropsychologists diagnose neurological and psychiatric disorders in patients with TBI. They evaluate the cognitive, behavioral, and psychological changes due to the history of TBI and other factors (e.g., co-morbid psychopathology) that can determine the persistence of cognitive deficits.
Studies on athletes evaluating the cognitive disorders that occurred after a sport-related injury, identify the groups at increased risk of concussion, such as boxing, football, and hockey players. Also, athletes have a better prognosis after TBI because they do not have pre-existing diseases or motivational problems, which can interfere with cognitive performance. Moreover, several observers evaluate athletes serially, emphasizing the tracking of cognitive changes [1].
Most patients with mild TBI quickly recover and will not remain with cognitive disorders. However, a small percentage will remain disabled, which is why the researchers tried to identify some negative prognostic factors, such as:
“Additive or cumulative” effect of recurrent concussion
Patients with a first concussion have a short-term disability after the trauma. This led to studying the cumulative effects among groups exposed to the risk of repetitive trauma (e.g., athletes and soldiers with multiple blast exposures). Chronic traumatic encephalopathy (CTE) is the term introduced to describe the neurological and cognitive changes occurring in patients with repetitive brain trauma, such as sleep disturbances, forgetfulness, and impaired cognitive function [1, 7].
Recent studies failed to identify a significant difference in cognitive disorders among patients with repetitive TBI compared to the general population. However, cortical changes (e.g., lower cortical thickness) have been identified in young and middle-aged populations, eventually leading to cognitive decline and dementia. Furthermore, the cognitive function evaluation tests showed a slight deterioration, more pronounced being the verbal fluency affected in the case of people with repeated TBI [8].
- The difference between “uncomplicated” and “complicated” mTBI is made through brain imaging (CT, MRI). Complicated mTBI is associated with intracranial changes (intraparenchymal hemorrhage) on brain imaging, and the evolution of these patients may follow the trajectory of those with moderate and severe forms of TBI more than those with uncomplicated mTBI.
- Pre-existing psychopathological disorders (anxiety, co-morbid depression, coincident stressors) lead to poor outcomes in mTBI patients [1].
Recovery patterns in military mTBI
Studies conducted on soldiers and veterans involved in the conflicts in Iraq and Afghanistan did not identify differences between cognitive disorders compared to the general population with concussions. However, the severity of brain trauma influences the prognosis of cognitive function to a greater extent than the injury mechanism. It was observed that pre-existing neuropsychological comorbidities and chronic pain are associated with poorer neuropsychological results after a TBI in both the military and civilian populations [1].
In the civilian population, the recovery of a patient after an uncomplicated contusion was established and they presented improvement in symptoms after a limited period. Unlike the civilian population, in the military population, the data on the evolution after mTBI of soldiers are of poorer quality. Researchers usually do not have access to emergency medical documents and cognitive status examinations. For this reason, only patient reports whose validity cannot be verified are used in re-evaluations of veterans with a history of TBI.
Factors such as exaggeration of symptoms, secondary injuries, and insufficient effort for recovery lead to the persistence of cognitive deficits beyond the expected period of combat-related concussion. Many times, the victims of a TBI will exaggerate their symptoms or feign cognitive impairments to obtain financial gain in the context of granting disability pensions.
The diagnosis of mild TBI is challenging for the clinician because the military frequently associates psychological disorders and PTSD in addition to head trauma. However, American researchers have identified a way to evaluate and treat veterans involved in the wars in Iraq and Pakistan using the Boston Assessment of Traumatic Brain Injury-Lifetime (BAT-L) algorithm. This score takes into account the number of blasts that took place within 100 m and to which the veteran was exposed, as well as the number of head injuries caused by an explosion.
In evaluating a TBI due to an explosion, cranial injuries that occurred before military service must be considered. For example, TBI that occurred in childhood can be more severe than injuries that occurred during a war. The impact of exposure to a blast in the absence of other traumas is not yet known [9].
Conclusion
Veterans with TBI represent a particular category of people due to the pre-existing neuropsychological conditions that resulted from participation in the war, to which TBI-related cognitive disorders are added. For this reason, the consequences of a TBI are difficult to assess in the veteran population, and an annual psychological assessment of military personnel is necessary [1].
In the literature, no significant differences were identified in the acute treatment and documentation of TBI patients from the civilian and military populations. However, a high level of variability in the results was observed, which is why the research was oriented toward identifying standardized measures such as functional outcomes through the quick return to work.
Identifying some biomarkers for estimating the level of disability of the patient after the acute period is the primary goal of the current studies. To achieve this goal, further research is needed to establish the strength of the clinical correlation [1].
For more information about the impact of TBI visit:
- Boston University Center for the Study of Traumatic Encephalopathy contribution to understanding this disease
- How does TBI affect the functions of patients?
- Advances in TBI care and therapies
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
Bibliography
- Lamberty GJ, Nelson NW, Yamada T. Effects and Outcomes in Civilian and Military Traumatic Brain Injury: Similarities, Differences, and Forensic Implications: Effects and outcomes of TBI. Behav Sci Law. 2013;31(6):814–32; doi: 10.1002/bsl.2091.
- Tenovuo O, Diaz-Arrastia R, Goldstein LE, Sharp DJ, et al. Assessing the Severity of Traumatic Brain Injury—Time for a Change? JCM. 2021;10(1):148; doi: 10.3390/jcm10010148.
- Adoni A, McNett M. The Pupillary Response in Traumatic Brain Injury: A Guide for Trauma Nurses. Journal of Trauma Nursing. 2007;14(4):191–6; doi: 10.1097/01.jtn.0000318921.90627.fe.
- Lee B, Newberg A. Neuroimaging in traumatic brain imaging. Neurotherapeutics. 2005;2(2):372–83; doi: 10.1602/neurorx.2.2.372.
- Rauch S, Marzolo M, Cappello TD, Ströhle M, et al. Severe traumatic brain injury and hypotension is a frequent and lethal combination in multiple trauma patients in mountain areas – an analysis of the prospective international Alpine Trauma Registry. Scand J Trauma Resusc Emerg Med. 2021;29(1):61; doi: 10.1186/s13049-021-00879-1.
- Dams-O’Connor K, Cantor JB, Brown M, Dijkers MP, et al. Screening for Traumatic Brain Injury: Findings and Public Health Implications. Journal of Head Trauma Rehabilitation. 2014;29(6):479–89; doi: 10.1097/HTR.0000000000000099.
- Theadom A, Parmar P, Jones K, Barker-Collo S, et al. Frequency and Impact of Recurrent Traumatic Brain Injury in a Population-Based Sample. Journal of Neurotrauma. 2015;32(10):674–81; doi: 10.1089/neu.2014.3579.
- List J, Ott S, Bukowski M, Lindenberg R, et al. Cognitive function and brain structure after recurrent mild traumatic brain injuries in young-to-middle-aged adults. Front Hum Neurosci. 2015;9; doi: 10.3389/fnhum.2015.00228.
- Fortier CB, Amick MM, Grande L, McGlynn S, et al. The Boston Assessment of Traumatic Brain Injury–Lifetime (BAT-L) Semistructured Interview: Evidence of Research Utility and Validity. Journal of Head Trauma Rehabilitation. 2014;29(1):89–98; doi: 10.1097/HTR.0b013e3182865859.




