Keywords: CENTER-TBI, TBI, outcomes, complicated mTBI, uncomplicated mTBI
Introduction
Before addresing the mild TBI outcomes we should focus first on the entire Traumatic brain injury (TBI) class, that continues to affect millions of individuals yearly all around the world. The overall incidence of TBI in the US between 2002-2006 was 579 per 100.000 persons, which means approximately 1.7 million cases per year. The hospitalization rate for these cases was 93.8 per 100,000 persons, compared to Europe, where the hospitalization rate was 235 per 100,000 persons, and it continued to increase worldwide in the decade 2001-2010 [1–2].
TBI remains one of the most important medical, societal, and healthcare problems influencing not only the lives of those affected but also their caregivers. Compared to the general population, people suffering from TBIs have more direct and indirect costs due to healthcare complications and loss of productivity in their daily lives [3].
Approximately 70-90% of the patients presenting to the hospital are diagnosed with mild TBI (mTBI), generally classified with a Glasgow Coma Scale (GCS) between 13-15. Previously, intracranial abnormalities found on computed tomography (CT) (depressed skull or trauma-related intracranial abnormalities) were used as a differentiation method. Still, the sensitivity of CT has improved over time, and an abnormal scan might no longer have the same significance as before [4].
Previous studies regarding the impact of complicated or uncomplicated mTBI on the patient’s outcome have been contradictory:
→ On the one hand, it was considered that the presence/absence of intracranial abnormalities might affect the prognosis, with complicated mTBI being associated with functional and cognitive outcomes comparable to those with moderate TBI that had a GCS between 9-13.
→ On the other hand, some studies showed that there was no relationship between complicated mTBI and functional and cognitive outcomes.
Moreover, there are divergent results in research concerning longitudinal outcomes after uncomplicated or complicated mTBI. Some studies expressed a worse outcome for patients with complicated mTBI, while others showed a better improvement and recovery in the case of patients after a complicated mTBI, while those suffering from an uncomplicated mTBI recovered slower. Some studies even revealed no significant difference between groups.
In the past, it was considered significant for the functional and neurocognitive outcome of the patient after a brain lesion and the post-concussive symptoms. In contrast, the health-related quality of life (HRQoL) is the most relevant for both the patient and the clinicians. HRQoL represents a person’s perception of how the illness and its treatment influence the mental, physical, social, and cognitive aspects of someone’s life.
Only a few studies evaluated the HRQoL outcomes in patients after uncomplicated or complicated mTBIs. Still, the differences between groups remain poorly understood. Large longitudinal studies comparing patients on different outcome categories (e.g., disease-specific and generic HRQoL and the presence/absence of post-traumatic stress and anxiety) are needed in the future. In addition, it is important to investigate the differences between groups using multidimensional approaches because the mTBI might affect different areas simultaneously.
The current research hypothesizes that patients suffering from a complicated mTBI have lower disease-specific and generic HRQoL and worse functional outcomes than those suffering an uncomplicated mTBI at three and six months.
Study design
The study analyzed patients from the Collaborative European NeuroTrauma Effectiveness Research (CENTER-TBI) research project, a multicenter, observational, prospective, longitudinal cohort study, conducted in Europe and Israel. Patients were included between December 2014 and December 2017.
The inclusion criteria were:
- a clinical diagnosis of TBI
- an indication of a CT scan
- presentation to a participating center within 24 hours from the time of the injury
- signed informed consent
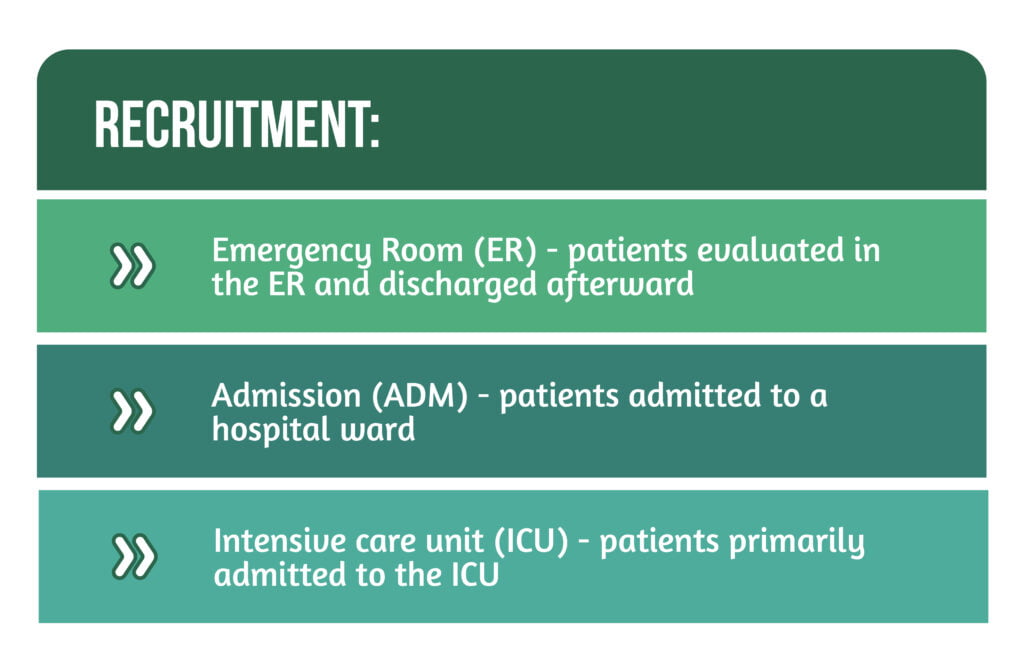
Patients were recruited on 3 strata, as shown in Figure 1.
Study Participants
Participants diagnosed with mTBI (GCS=13-15) were included and differentiated into two groups: uncomplicated and complicated mTBI, using the absence/presence of any intracranial abnormality on the first CT scan.
The presence of an intracranial abnormality was defined as the detection of ≥1 finding on the CT scan (Figure 2).
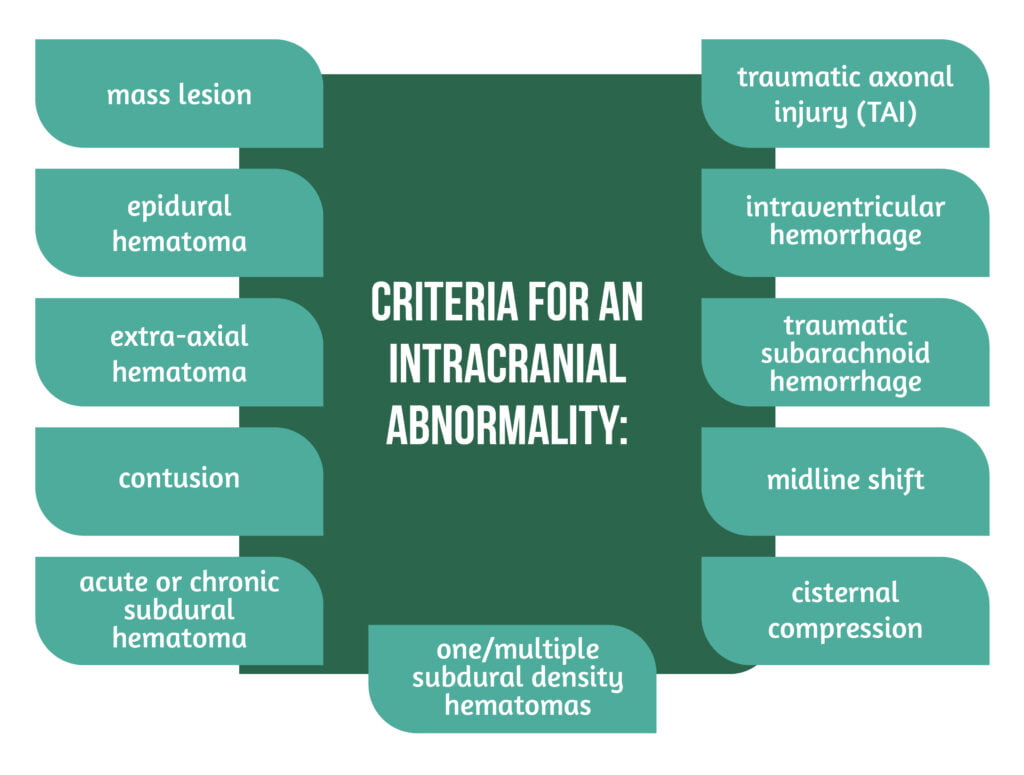
A linear or depressed skull fracture in the absence of any other structural intracranial abnormality was not considered a criterion for complicated mTBI. Moreover, participants had to be older than 16 years and classified with a GOSE ≥3.
In order to assess individuals’ health status before the injury, the American Society of Anesthesiologists Physical Status Classification System (ASA-PS) was used. For all analyses, the variables were analyzed at three and six months.
Instruments
Seven instruments were used to measure and assess the outcomes of patients.
-
HRQoL
For the generic HRQoL, the 36-item Short Form Health Survey (SF-36v2) was used. The questionnaire comprises 36 items covering 8 domains and applies different response scales. The total score ranges from 0 to 100, with higher values indicating higher HRQoL, and scores under 40 are considered impaired.
For disease-specific HRQoL, the Quality of Life after Brain Injury (QOLIBRI), a 37-item self-report instrument, was used in order to determine the level of satisfaction with different aspects of TBI-specific HRQoL. Higher values indicate a better HRQoL. For the QOLIBRI, a score under 60 is considered impaired.
-
Functional Outcome
The Glasgow Outcome Scale – Extended (GOSE) was used in order to measure the outcome after the TBI. The functional outcome was rated by the clinician on an 8-point scale (Figure 3).
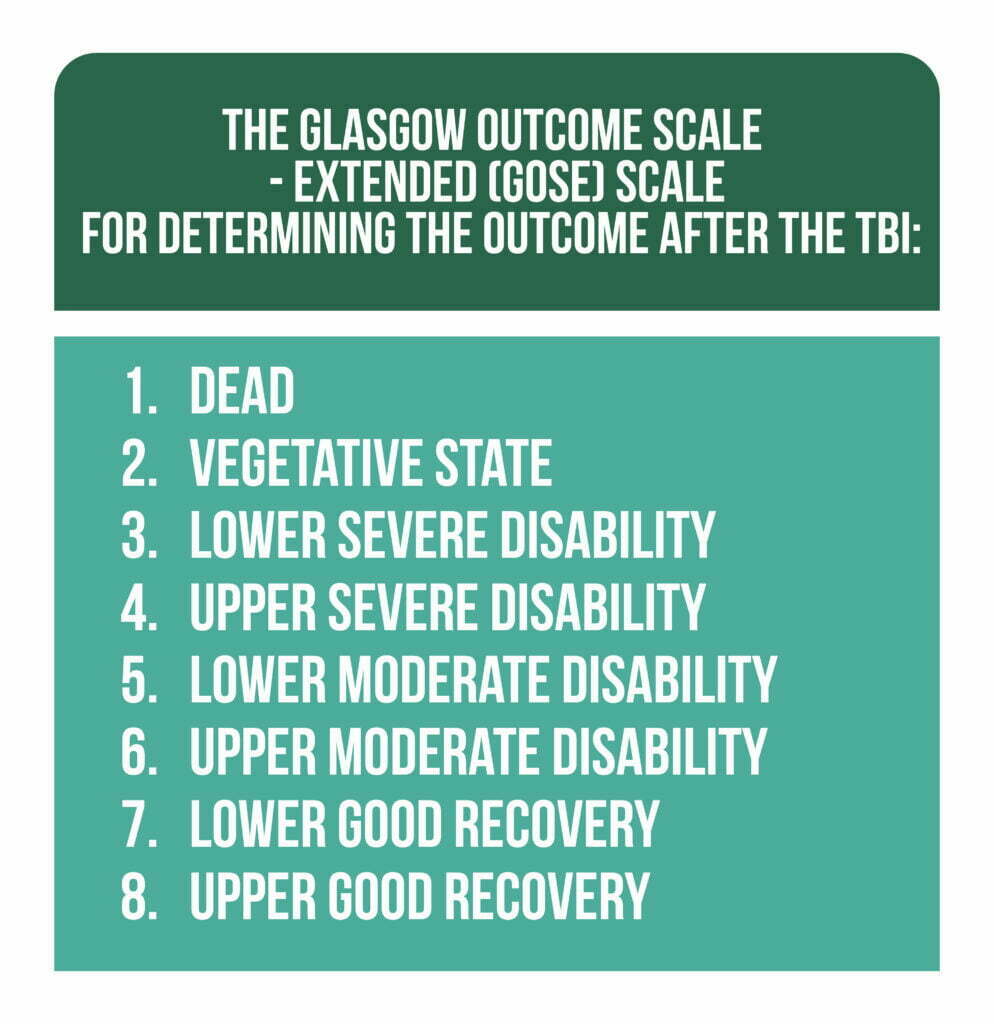
In the current research, a GOSE score ≤6 was considered impaired. Patients with GOSE 1 were excluded from the analyses, and those with GOSE 2-3 were collapsed into one.
-
Post-Traumatic Stress, Depression and Anxiety
For measuring PTSD, the Post-traumatic Stress Disorder Checklist-5 (PCL-5) was used. It measures 20 symptoms of the disorder based on the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-V). It uses a five-point scale, and a score ≥33 (from a total of 80) is considered to be clinically relevant.
Depression symptoms were evaluated using the Patient Health Questionnaire (PHQ-9), a nine-item instrument used for self-assessment. The maximum score is 27, and the higher the score obtained by the patient, the higher the indication that they might be suffering from depression.
The Generalized Anxiety Disorder questionnaire was used for evaluating anxiety, with a total score of 27. A score above 10 was generally considered an indicator of anxiety disorder in the patient.
Outcomes and Discussions
A total of 2955 patients were included in the CENTER-TBI cohort after mTBI, and the study sample was formed of 1104 patients at 3 and 6 months after the mTBI. The complicated (51.5%) to uncomplicated mTBI (48,5%) ratio was almost equal. Of the total number of patients admitted, 30.6% were through the ER, 47.6% were admitted to a ward, and 21.8% were admitted directly to the ICU. The majority of patients suffered the injury after a fall (47%) or after a traffic accident (39%). Approximately 11% of the patients reported suffering a TBI previous to the current injury.
The study focused on the outcome of patients with uncomplicated and complicated mTBI at 3 and 6 months post-injury. A better understanding of the relationship between these two categories might improve intervention and rehabilitation strategies.
Patients who suffered a complicated injury had lower generic and disease-specific HRQoL and worse functional outcomes at both times they were evaluated. In addition, the cut-off for mild depressive symptoms was reached at 3 months post-injury in patients with a complicated mTBI, which indicates the need for an appropriate follow-up and early treatment.
Ponsford et al. revealed in their study that no significant difference in psychiatric functionality was found comparing mTBI patients with control groups at 7 months post-injury. However, memory and concentration might be impaired. Also, they suggested that the majority of individuals make a good recovery 7 months post-TBI when focusing on depression/anxiety, post-concussion symptoms, and physical quality of life scores [5].
Lessons from CENTER-TBI
The current study is unique due to the large number of patients and the comparison of patients on different outcome levels (e.g., functional outcome, generic and disease-specific HRQoL, and symptomatology). In addition, the multivariate statistical approach further strengthens the results obtained. The method especially combines information from multiple outcome measures and is suitable for non-normal data.
There are several limitations to the current research that need to be taken into account (1) coping and resilience were not measured, (2) their impact that on the outcome was not measured. Keeping in mind that magnetic resonance imaging has a higher sensitivity and has proven preferable tool when assessing a TBI patient, Williams’ classification of complicated vs. uncomplicated mTBI might underestimate the presence of brain abnormalities due to the injury. In addition, the post-injury treatment has not been accounted for, even though it might influence the outcome and recovery course of the patient. Finally, a response bias might also be present because patients with lower functional outcomes and HRQoL might be more inclined to participate.
Future research should focus on patient follow-up at 5 and 10 years post-injury. Also, studies into biomarkers and specific localization of injury using CT or magnetic resonance imaging scans can help refine the conclusions of this study. Moreover, results from the current research should be compared to patients with non-brain injured trauma and to the general population.
Conclusions | Mild TBI outcomes
The study of Ponsford et al. indicates that patients after a complicated mTBI have lower generic and disease-specific HRQoL and worse functional outcomes than those suffering from an uncomplicated mTBI at 3 and 6 months post-injury. However, the differences were small between the groups, and significant baseline differences between some measures might have contributed to these findings.
In the future, clinicians, patients, researchers, and decision-makers in health care should concentrate on the long-term outcomes and effects for these patients after suffering from mTBI. Therefore, tailored therapy should be provided as soon as possible for these patients in order to improve as much as possible their HRQoL and their psychosocial and psychological outcomes.
For more information about the impact of TBI visit:
- TBI impact on relationships
- The importance of prehospital care for severe TBI
- How does TBI affect sleep?
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
Bibliography
- Faul M & Coronado V. Epidemiology of traumatic brain injury’, Handb. Clin. Neurol., vol. 127, pp. 3–13, 2015, doi: 10.1016/B978-0-444-52892-6.00001-5.
- Galgano M, Toshkezi G, Qiu X, Russell T et al. Traumatic Brain Injury: Current Treatment Strategies and Future Endeavors. Cell Transplant. 2017, vol. 26, no. 7, pp. 1118–1130. doi: 10.1177/0963689717714102.
- Majdan M et al. Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis. Lancet Public Health 2016, vol. 1, no. 2, pp. e76–e83. doi: 10.1016/S2468-2667(16)30017-2.
- Voormolen DC et al. Outcomes After Complicated and Uncomplicated Mild Traumatic Brain Injury at Three- and Six-Months Post-Injury: Results from the CENTER-TBI Study. J. Clin. Med. 2020, vol. 9, no. 5, p. 1525. doi: 10.3390/jcm9051525.
- Ponsford J, Cameron P, Fitzgerald M, Grant M, and Mikocka-Walus A. Long-term outcomes after uncomplicated mild traumatic brain injury: a comparison with trauma controls. J. Neurotrauma 2011, vol. 28, no. 6, pp. 937–946. doi: 10.1089/neu.2010.1516.




