Authors: Luis Rafael Moscote-Salazar 1, Tariq Janjua 2, Murli Manju 3, William A. Florez-Perdomo 4, Amit Agrawal 5
Affiliations:
- Colombian CLinical Research Group in Neurocritical Care, Colombia
- Department of Neurology, Regions Hospital, Saint Paul, MN, icumd@outlook.com
- Department of Anatomy, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India
- Colombian CLinical Research Group in Neurocritical Care, Colombia
- Department of Neurosurgery, All India Institute of Medical Sciences, Saket Nagar, Bhopal 462020, Madhya Pradesh (India), email- dramitagrawal@gmail.com.
Correspondence: Luis Rafael Moscote-Salazar MD, E-mail: rafaelmoscote21@gmail.com
Keywords: Hypothermia, traumatic brain injury, temperature
Introduction – Hypothermia as a neuroprotective strategy after TBI
Temperature is a physical parameter, and an excessively high (hyperthermia) or low temperature (hypothermia) can alter metabolic rates and cause organ damage [1]. The brain executes multiple processes, which are dependent on energy expenditure, even at rest [2,3]. Hence, the brain is the most metabolically active organ in humans, representing between 25% of glucose metabolism and 20% of the total body oxygen consumption [3,4].
Human beings are homeothermic mammals that need to maintain a core body temperature in the range of 36–37.5°C [5]. Any deviations above or below these values translate into notable enzymatic, cellular, and tissue dysfunctions [4,6]. Brain temperature is correlated with and slightly higher than core body temperature, and the mean gradient ranges from 0.3°C to 1.1°C [4,7].
The brain’s temperature depends, to a large extent, on the added effects of the variables [2,5] showcased in Figure 1.
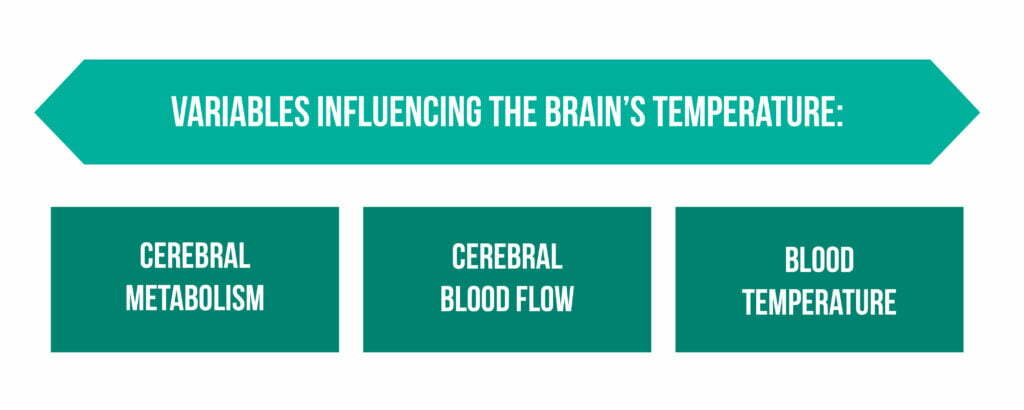
Further anatomical features can alter the brain’s temperature. These include [5,8]:
- the structure of the layers of the scalp (diploic skull bone, soft tissue, and meningeal coverings)
- gender
- age
- exercise
- stress
- diet
- time of day
- drugs
The temperature control or thermostat function is performed in the hypothalamus, and it helps in maintaining the proper temperature in the physiological range [9].
Hyperthermia and brain
Hyperthermia in neurocritical patients, particularly in patients with severe head injury, can aggravate the inflammatory cascade and thus increase the risk of secondary brain injury [6, 9–10]. It is suggested that patients with brain injuries or cardiac arrest can benefit from neuroprotection and therapeutic hypothermia, increasing the chances of survival and improved neurological outcomes [11].
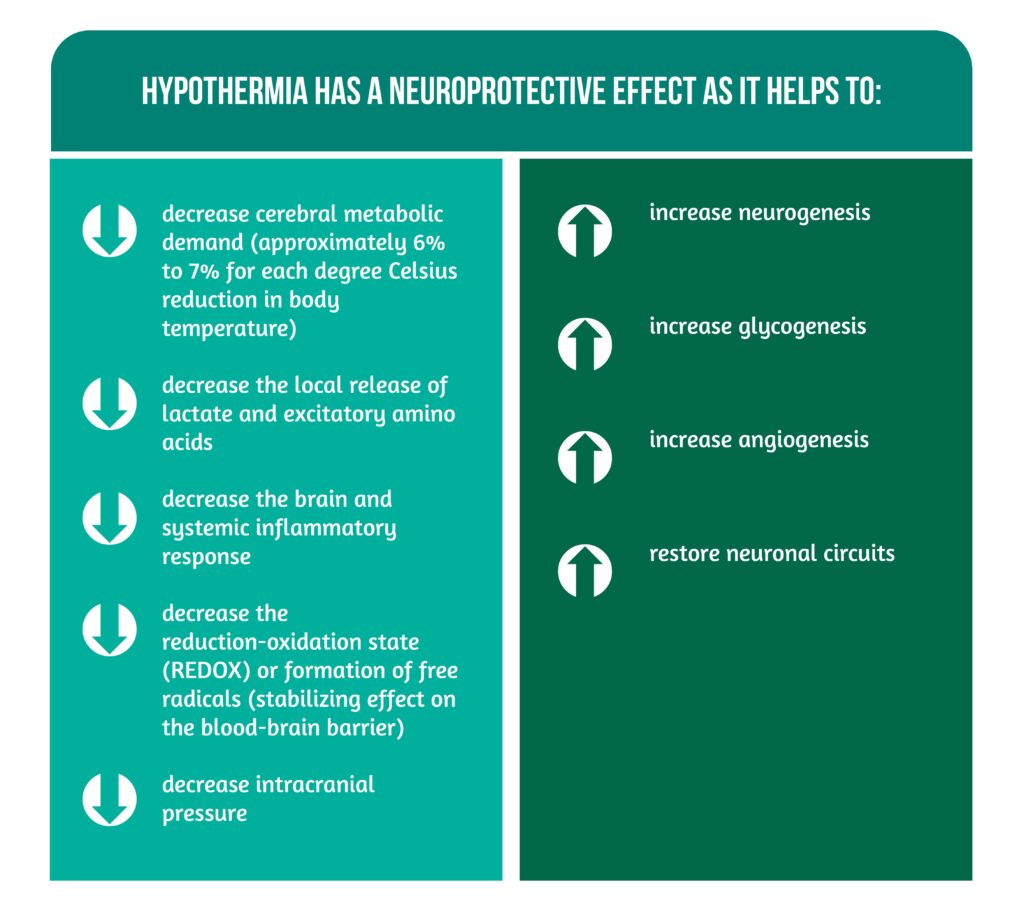
Hypothermia has a neuroprotective effect as it helps in the processes described in Figure 2 [3, 6–7, 9, 12-14].
Hypothermia
For centuries, total or partial cooling has been used sporadically to preserve neuronal viability and improve outcomes, including functional recovery [12,14]. When the body temperature is lower than 36.5 ºC, it is considered hypothermia [3]:
- mild hypothermia – temperature range: 33–36°
- moderate hypothermia – temperature range: 28–32°C
- profound hypothermia – temperature <28°C [15,16].
In mild hypothermia, the body reacts with thermoregulatory mechanisms, such as shivering and vasoconstriction; however, as the degree of hypothermia progresses, the body has physiological changes that can be fatal [6]. For this reason, continuous monitoring of core body temperature is essential to ensure that mild hypothermia is maintained and to avoid unwanted side effects [17].
Clinical implications
Core body temperature is measured from central body sites, such as the lower end of the esophagus, nasopharynx, urinary bladder, and pulmonary artery, the latter being considered the best measure of core temperature [7,17]. However, these invasive methods are reserved for intensive care units, and in clinical practice, measurement by non-invasive techniques is usually sufficient, as it can be performed within the oral cavity, rectum, axilla, and ear as the most commonly used sites, although they are not recommended to monitor the temperature during the advanced cooling period because these measurements are inaccurate [2,3].
The therapeutic use of hypothermia represents a protective factor in cases of brain injuries, which is why it has been used in cases of both patients with cardiac arrest and neonatal hypoxic-ischemic encephalopathy [7]. As for other types of neurological injuries (e.g., cerebrovascular accidents and injuries of a traumatic nature), the effectiveness of this method has not been completely established [18].
Therapeutic options
Many therapeutic methods have been described in the literature. Some are not used due to their ineffectiveness or because they are not viable. Other methods are not effective if administered individually, such as the exclusive use of antipyretic drugs, which is not enough to achieve an ideal treatment [19]. Similarly, in the absence of electrical sources, intravenous cold crystalloid is useful to initiate hypothermia at the prehospital level; however, a large volume is needed for the induction phase [9].
Studies conclude that ideal therapy cannot be attained with cold fluids alone and that cooling helmets or hoods are effective in achieving selective brain thermal treatment in infants but appear to be ineffective in adults [19].
Core challenges
When inducing hypothermia in a patient, several issues must be considered, such as [18]:
- What cooling method to use?
- Will it be easy to implement this in that patient?
- How safe and tolerable will that patient be when inducing hypothermia?
- How fast will the target be reached?
- How long will the cooldown last?
- What complications or adverse events will the patient experience?
According to each phase of the TTM, adverse events are presented. Therefore, during the induction phase, both tremors and hypovolemia, hyperglycemia, electrolyte alterations, and hypercapnia can occur; during the maintenance phase, infections might be present, and in the last phase, hyperglycemia, hyperkalemia, or reperfusion injury may arise [16]. Fisher M et al. [10] supported that there was still no general recommendation for using hypothermia due to the adverse events that could occur, such as cardiac arrhythmias, uncontrollable tremors, thromboembolism, and even infections. Tokutami T et al. [20] also referred to the adverse effects of hypothermia at a temperature <35°C, describing that hypothermia below that range predisposes patients to persistent cumulative O2 debt.
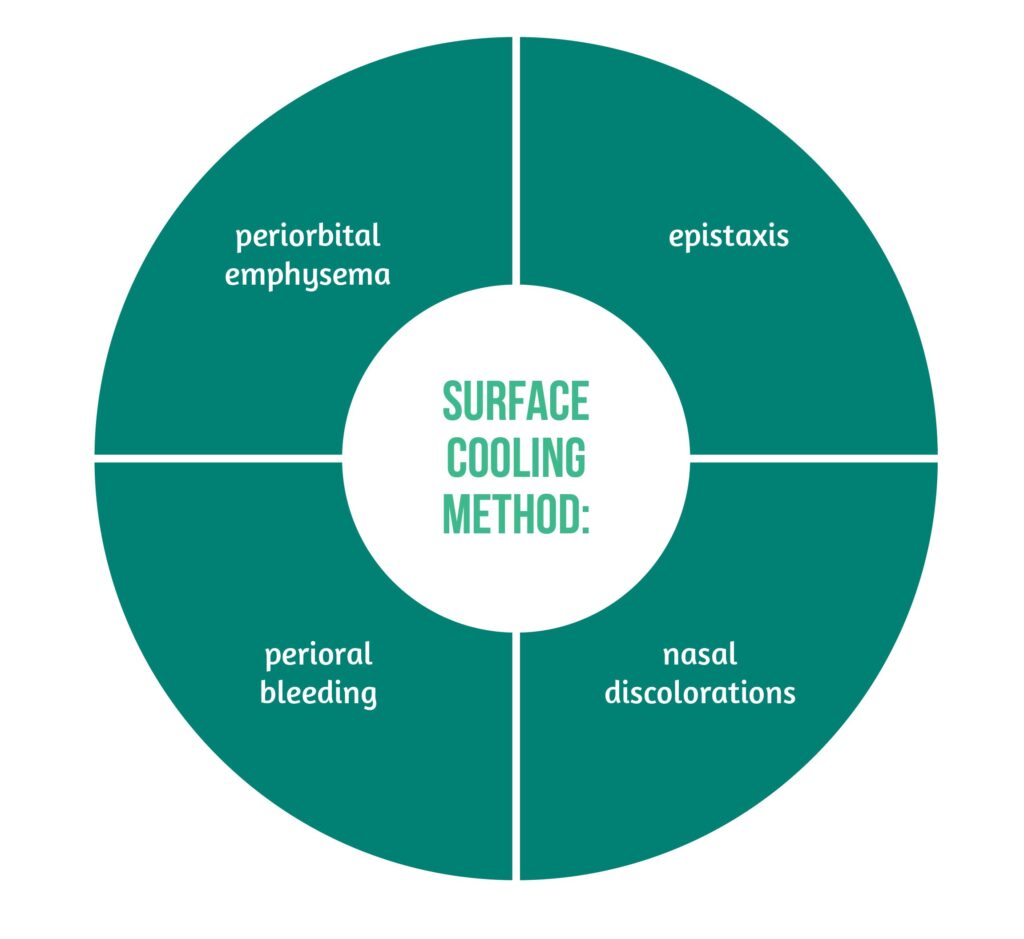
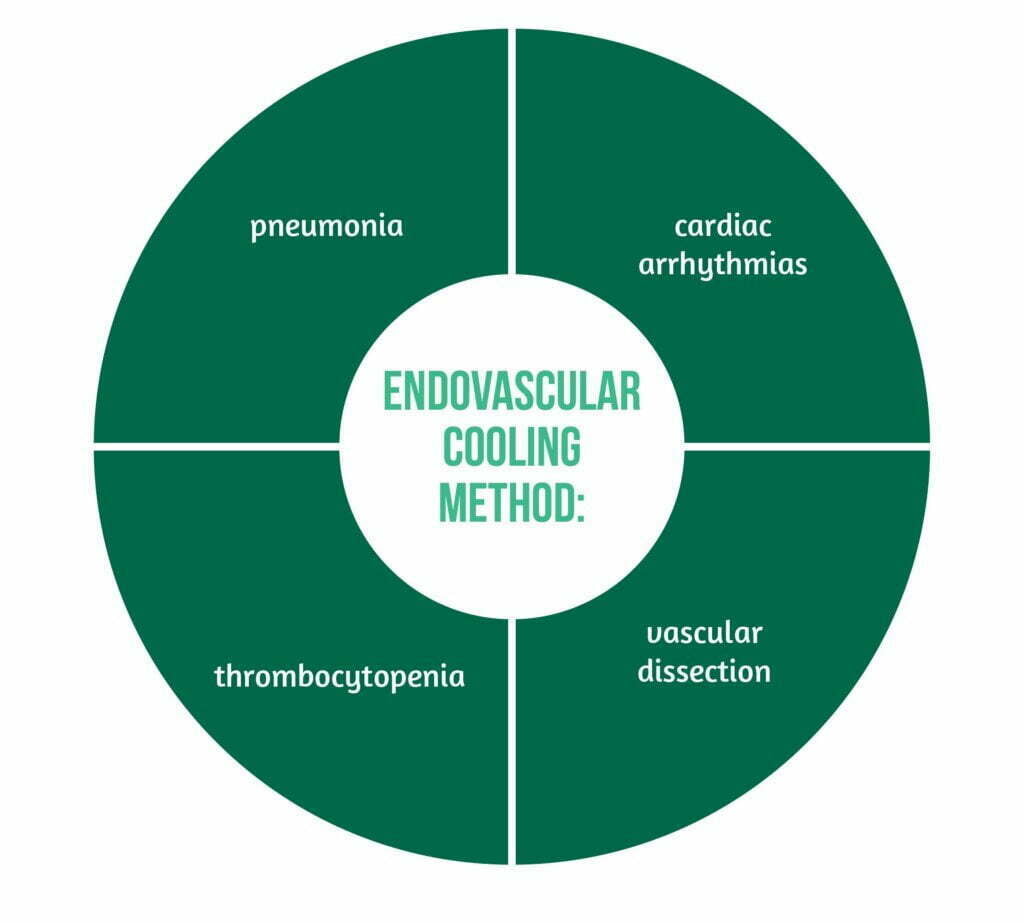
Patients treated with the surface cooling method, according to the research by Song et al., presented the adverse events showcased in Figure 3, while patients who used the endovascular cooling method, adverse events included those presented in Figure 4 [18].
Summary
In summary, therapeutic hypothermia in recent years has been established as a neuroprotective method. However, its use in brain injuries or post-cardiac arrest has not been fully elucidated since there are still obstacles to its use, which can be overcome by the establishment of guidelines and integrating a multidisciplinary team that is necessary to successfully implement a cooling protocol. There are still limitations that do not allow the use of hypothermia as a treatment, such as a lack of knowledge and controversies about the most effective method to reach the target temperature.
For more insight into TBI, visit:
- VENTILatOry Strategies in TBI: New Avenues for Acute Respiratory Distress Syndrome (ARDS) patients
- Prevention of Neurotrauma is the Best Treatment
- Neurotrauma and Info-pollution: A call for action
References
- Ruiz, MNS, JM García, and BM Fernández. Body temperature and its importance as a vital constant. Revista De Enfermeria (Barcelona, Spain), 2009. 32(9): p. 44-52. Available at: https://pubmed.ncbi.nlm.nih.gov/19839238/
- Mrozek S, F Vardon, and T Geeraerts. Brain Temperature: Physiology and Pathophysiology after Brain Injury. Anesthesiology Research and Practice 2012. 2012: p. e989487. DOI: 10.1155/2012/989487
- Rincon F. Targeted Temperature Management in Brain Injured Patients. Neurol Clin, 2017. 35(4): p. 665-694. DOI: 10.1016/j.ncl.2017.06.005
- Wang H, et al. Brain temperature and its fundamental properties: a review for clinical neuroscientists. Frontiers in Neuroscience, 2014. 8: p. 307. DOI: 10.3389/fnins.2014.00307
- Wang H, et al. Thermal Regulation of the Brain—An Anatomical and Physiological Review for Clinical Neuroscientists. Frontiers in Neuroscience, 2016. 9. doi: 10.3389/fnins.2015.00528
- Karnatovskaia, LV, KE Wartenberg, and WD Freeman. Therapeutic hypothermia for neuroprotection: history, mechanisms, risks, and clinical applications. The Neurohospitalist, 2014. 4(3): p. 153-163. DOI: 10.1177/1941874413519802
- Bindra A and D Gupta. Targeted temperature management in neurocritical care: Boon or bust. Journal of Neuroanaesthesiology and Critical Care, 2016. 03(02): p. 096-109. DOI: 10.4103/2348-0548.182330
- Garami A and M Székely. Body temperature: Its regulation in framework of energy balance. Temperature: Multidisciplinary Biomedical Journal, 2014. 1(1): p. 28. DOI: 10.4161/temp.29060
- Muengtaweepongsa S and W Srivilaithon. Targeted temperature management in neurological intensive care unit. World Journal of Methodology, 2017. 7(2): p. 55. doi: 10.5662/wjm.v7.i2.55
- Fischer M et al. Keep the brain cool—endovascular cooling in patients with severe traumatic brain injury: a case series study. Neurosurgery, 2011. 68(4): p. 867-873. DOI: 10.1227/NEU.0b013e318208f5fb
- Kallmünzer B and R Kollmar. Temperature management in stroke – an unsolved, but important topic. Cerebrovascular Diseases (Basel, Switzerland), 2011. 31(6): p. 532-543. DOI: 10.1159/000324621
- Palencia Herrejón, E. and D. Díaz Díaz, Therapeutic hypothermia: Time for a moratorium. Med Intensiva, 2017. 41(7): p. 425-428. DOI: 10.1016/j.medin.2017.04.003
- Cariou A, et al. Targeted temperature management in the ICU: guidelines from a French expert panel. Ann Intensive Care, 2017. 7(1): p. 70. doi: 10.1186/s13613-017-0294-1.
- Tapia-Velasco R. Therapeutic hypothermia. Revista Mexicana de Anestesiología, 2015. 38(S3): p. 449-451.
- Karcioglu O, et al. A systematic review of safety and adverse effects in the practice of therapeutic hypothermia. The American Journal of Emergency Medicine, 2018. 36(10): p. 1886-1894. doi: 10.1016/j.ajem.2018.07.024
- Saigal S. et al. Targeted temperature management: Current evidence and practices in critical care. Indian J Crit Care Med, 2015. 19(9): p. 537-46. doi: 10.4103/0972-5229.164806.
- Stauffer PR, et al. Non-invasive measurement of brain temperature with microwave radiometry: demonstration in a head phantom and clinical case. Neuroradiol J, 2014. 27(1): p. 3-12. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4066964/
- Song SS and PD Lyden. Overview of Therapeutic Hypothermia. Current treatment options in neurology, 2012. 14(6): p. 541-548. doi: 10.1007/s11940-012-0201-x.
- Miñambres E et al. [Therapeutic hypothermia in neurocritical patients]. Med Intensiva, 2008. 32(5): p. 227-35. doi: 10.1016/s0210-5691(08)70945-8.
- Tokutomi T, et al. Effect of 35 degrees C hypothermia on intracranial pressure and clinical outcome in patients with severe traumatic brain injury. The Journal of Trauma, 2009. 66(1): p. 166-173. doi: 10.1097/TA.0b013e318157dbec.