Keywords: TBI, stiffness, weakness
Introduction | How does TBI affect spasticity?
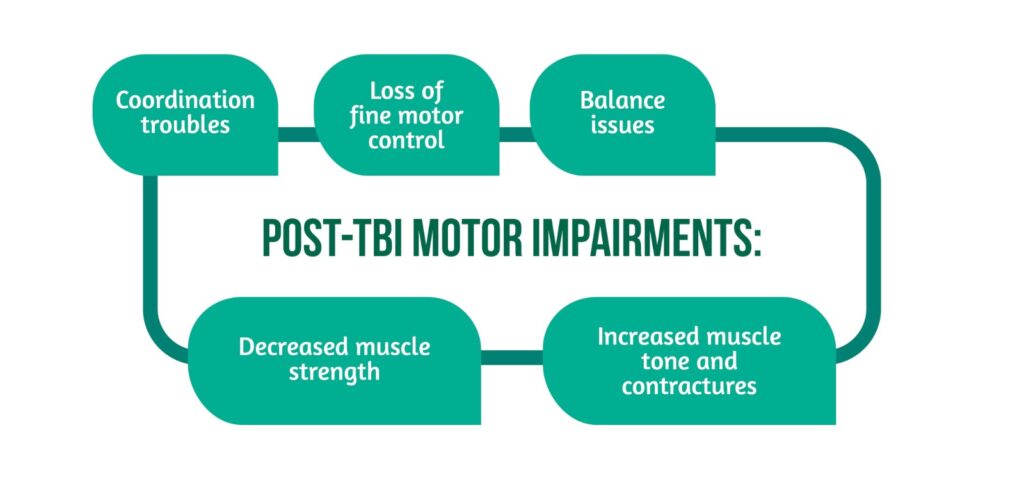
Traumatic brain injury (TBI) occurs frequently in the general population and leads to long-term consequences, such as cognitive, psychological, and motor impairments which decrease the quality of life. Nowadays, TBI is increasingly recognized as a chronic disease. Recent studies showed that besides acute motor deficits, a severe TBI increases the risk of long-term neurodegenerative diseases, such as Parkinson’s disease and amyotrophic lateral sclerosis [1]. After a moderate or severe TBI, many patients are going to have motor impairments (Figure 1) [2].
All these disturbances affect independence and can lead to psychological problems. This, in turn, can make patients unable to work, decreasing the labor force, and increasing society’s expenses [2].
What is spasticity?
Spasticity represents the stiffening of muscles caused by damaging the nervous fibers between the brain and muscles, due to a TBI. As a result, the muscles become contracted, and patients cannot stretch or relax them [3].
The manifestations include:
- Muscle weakness – affects the ability to walk independently.
- Loss of fine motor control – fine motor control helps people to pick up small objects with their fingers.
- Exaggerated deep tendon reflexes.
- Muscle spasms – represent painful involuntary muscle contractions that can appear after a light touch.
- Involuntary crossing of the legs (scissoring).
- Muscle and joint deformities – patients experience stiff muscles without the ability to relax. After a variable period with stiff muscles, joint deformities will appear [2,3] (Figure 2).

What you should know about spasticity?
Spasticity is an early onset symptom, as it appears soon after a TBI, often after one week, and has variable intensity: After a TBI some people do not develop spasticity, while others have mild or even severe forms. Patients with severe TBI have more chances to have increased spasticity. For some patients, it significantly impacts their quality of life.
The affection can present with fluctuating symptoms, meaning it gets worse when the patient does physical activity or during the night.
Severe spasticity is almost permanent and debilitating for the patient.
When considering treatment for spasticity, patients should learn which kind of moves they should avoid. Moreover, some of them will need medicines for symptom relief. Focal spasticity (which affects only a few muscles) can be treated locally by botulinum toxin injections or nerve blocks [3].
What triggers spasticity?
A patient can feel spastic all the time, but some factors that can increase spasticity:
- Movements or stretching of the extremities.
- Bladder problems – When experiencing pain during urination, an unpleasant smell of the urine, or a new onset frequent need to go toilet, these are the signs of a urinary infection which can increase the stiffness. It is very important to take a sample of urine for laboratory testing and go to a general practitioner (GP) [5].
- Bowel problems – Constipation is another factor that can aggravate spasticity. If you have trouble with moving your bowels, hard stools, difficulties passing, or large hemorrhoids, these are the signs to go to a GP for further investigations and treatment.
- Skin affections – Excessive pressure on the skin affects circulation, leading to skin lesions that cause moving difficulties. It is essential to avoid tight clothing, friction from new footwear, or sun exposure.
- Infections – Every kind of infection such as teeth, respiratory, or urinary, is going to aggravate the spasticity. Therefore, they require urgent addressing.
- Emotional issues, excessive fatigue, and extreme temperatures can temporarily worsen the symptoms [3,5].
When should spasticity be treated?
Spasticity is not problematic in all instances, but there are some cases when it is harmful and debilitating, and interacts with a patient’s independence.
There are some problems caused by stiffness which can be treated or prevented with appropriate medication:
- Pain when stretching the muscles.
- Limited mobility of the joints, which negatively impacts moving or walking.
- Inability to stay comfortable in bed, chair, or wheelchair.
- Frequent falls.
- Inability to sleep during the night and tiredness during the day.
- Skin pressure ulcers.
- Inability to perform daily activities such as feeding, bathing, or grooming.
How can spasticity be improved?
Firstly, it is important to avoid triggers by maintaining good hygiene, wearing loose clothes, treating urinary infections, eating fiber, drinking a lot of water, and wearing splints [3].
- Certain physical treatments alleviate spasticity [3]:
- Stretching exercises – help to maintain or improve joint mobility
- Positioning techniques (e.g., orthoses, splints) help to stretch muscles and increase mobility
- Standing with support – helps to unbend muscles and improve weakness.
Other therapeutic options include those showcased in Figure 3.

- Cryotherapy: helps to reduce the resistance of stiff muscles and decrease clonus by applying cold packs, usually for 20 minutes. This therapy also has a temporary analgesic effect (weeks to months) but without any change in proprioception deficits. The effects are due to lowering muscle temperature which reduces nerve activity and muscle tension [6,7].
- Thermotherapy: leads to muscle relaxation by changing motor neuron excitability. The exposure to high temperatures is done in a controlled environment by bathing in hot water or using a sauna [7].
- Infra-red heat increases the superficial body temperature, activates blood circulation, increases metabolism, and promotes muscle relaxation. It also plays a role in pain relief [7].
- Hydrotherapy involves using water to relieve pain and stiffness. Water has multiple benefits for the human body in many diseases. It promotes psychological relaxation, decreases joint overload, and helps to increase mobility [6].
What therapies relieve spasticity?
Nowadays there are many types of interventions for relieving spasticity which are chosen by the doctors according to the presence of focal or systemic symptoms, and taking into account the patient’s comorbidities.
Several drugs are used to improve generalized spasticity. However, as all medications can present side effects, spasticity drugs can cause sleepiness or weakness. For this reason, it is important to consider if the benefits outweigh the adverse effects [3]. Common medication options are presented in Table 1.
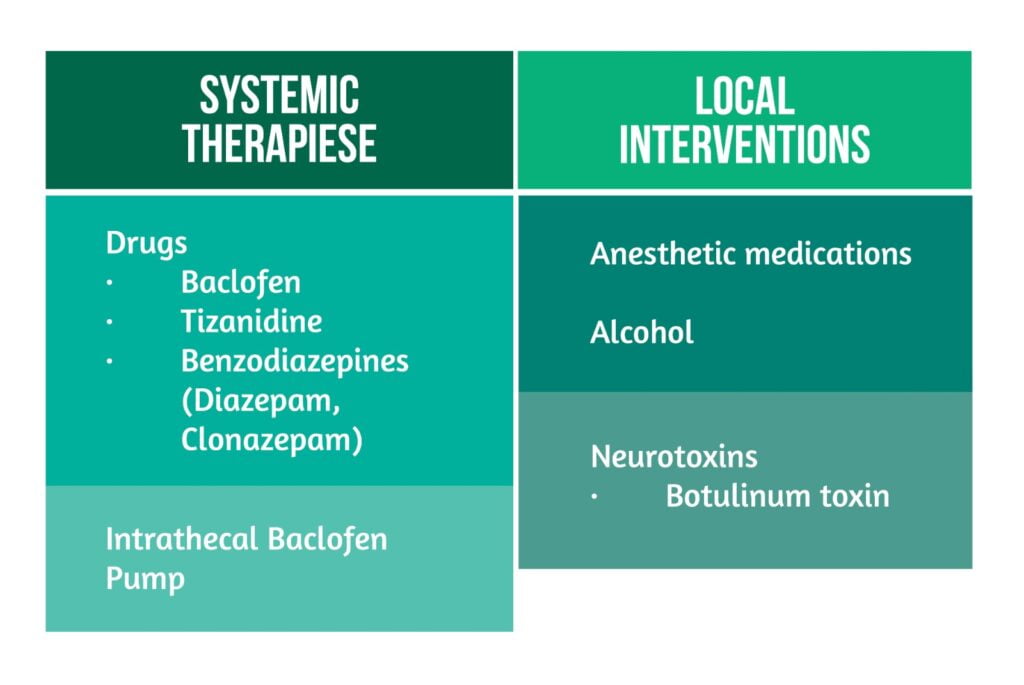
The oral form of baclofen is considered the first-line treatment for many patients with spasticity, but high doses are often required for better results. This increases the risk of adverse reactions, such as drowsiness, sedation, and systemic muscle relaxation, the reason why the medicine is not recommended for the elderly. The discontinuation of baclofen treatment is done gradually to avoid withdrawal symptoms such as confusion, hyperthermia, or seizures [8].
In some cases with severe stiffness where drugs have no significant effect, an intrathecal baclofen pump is a more suitable therapeutic intervention. This pump administers the medicine directly at the spinal level through a spinal catheter, allowing for higher central doses of baclofen and fewer systemic side effects. The advantage of this method is the possibility of titrating the doses according to the daily needs of the patient, thus ensuring as much mobility as possible and nocturnal spasms can be avoided.
* Pump failure can lead to the release of a large amount of medicine with the relaxation of the respiratory muscles and coma, or the occurrence of withdrawal symptoms in the case of the lack of release of the drug [3,8].
Botulinum toxin is a substance produced by Clostridium botulinum which is used for focal spasticity treatment to avoid sedation and generalized weakness. The toxin is injected in affected muscles, after performing an electromyography that helps to accurately identify the affected nerve. Studies showed that Botox is better tolerated and is more efficient than oral therapy. Moreover, the effects of botox are reversible, and they last 3-4 months. The most feared adverse effect is dissemination to other areas of the body (e.g. dysphagia may occur after injection in the neck or upper limbs) [3,8].
Alcohol or other substances are injected perineurally to relieve spasticity by destroying the affected nerve irreversibly. This treatment method is nonselective, it’s impossible to inject only the affected nerve, and the effects are variable ranging from days to years due to the nerve’s ability to regenerate. Currently, this method is used only for refractory spasticity to other more noninvasive therapies or for bedridden patients, who are not able to move their lower limbs or to feel any touch, as a palliative therapy to reduce muscle pain and stiffness. [8].
Conclusion
Spasticity is a debilitating condition that can affect TBI patients in different ways leading to lifelong physical, emotional, and behavioral changes. Moreover, it plays a role in reducing the patient’s quality of life and can have a significant impact on his family or caregiver(s). Spasticity after a TBI is an intensively researched topic, but there are still not enough studies to determine the long-term effects of a TBI. Primary prevention remains the key element for avoiding a trauma and its immediate complications, as well the long-term disabilities.
For more information about the impact of TBI visit:
- Assessment of Quality of Life after TBI using QOLIBRI-OS
- Can TBI affect taste and smell?
- TBI outcomes in Europe
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
Bibliography
- Corrigan F, Wee IC, Collins-Praino LE. Chronic motor performance following different traumatic brain injury severity—A systematic review. Front Neurol. 2023;14:1180353. doi:10.3389/fneur.2023.1180353
- Traumatic Brain Injury: effects on the brain and motor coordination | Noldus. Traumatic Brain Injury: effects on the brain and motor coordination | Noldus. Available from: https://www.noldus.com/blog/tbi-effects-brain-motor-coordination
- Spasticity and Traumatic Brain Injury. Available from: www.msktc.org/tbi/factsheets
- What is Adult Spasticity – Dysport® (abobotulinumtoxinA) | Dysport. Available from: https://www.dysport.com/en-us/adult-spasticity/about-adult-spasticity
- Trust MS. Spasticity triggers. MS Trust. Available from: https://mstrust.org.uk/a-z/spasticity/spasticity-triggers
- Blanchette AK, Demers M, Woo K, Shah A, et al. Current Practices of Physical and Occupational Therapists Regarding Spasticity Assessment and Treatment. Physiotherapy Canada. 2017;69(4):303-312. doi:10.3138/ptc.2016-54
- Monaghan K, Horgan F, Blake C, Cornall C, et al. Physical treatment interventions for managing spasticity after stroke. Cochrane Stroke Group, ed. Cochrane Database of Systematic Reviews. 2017. doi:10.1002/14651858.CD009188.pub2
- Chang E, Ghosh N, Yanni D, Lee S, et al. A Review of Spasticity Treatments: Pharmacological and Interventional Approaches. Crit Rev Phys Rehabil Med. 2013;25(1-2):11-22. doi:10.1615/CritRevPhysRehabilMed.2013007945