Keywords: TBI, CENTER-TBI, fatigue
Introduction on fatigue frequency after TBI
Traumatic brain injury (TBI) is a very important public health, medical and societal issue worldwide nowadays. It represents a major cause of mortality and morbidity, especially in young people, but the incidence is also increasing in persons older than 65 years, most significantly in high-income countries. Research shows that the highest rate of TBIs seems to be in the 0 to 4 years old group as well as in adolescents and young adults (15-24 years old), followed by another peak in the elderly (above 65 years) as mentioned above [1]. Among survivors, it is a significant cause of long-term disability, influencing their lives and the lives of their family, relatives, and friends. Compared to the general population, brain injury patients have a decreased life expectancy and increased mortality, and also, it is well known that TBI patients incur important direct and indirect costs [1]. Find out how can TBI affect ballance.
Research shows that each year there are an estimated 235,000 hospitalizations for nonfatal TBIs in the United States, with 1.1 million patients being treated in the emergency department and then released. Approximately 50,000 patients suffering from a TBI die annually due to injury or its consequences. It is considered that the annual incidence of TBI is 506,4 per 100,000 people in the United States. It is clear that this pathology remains one of the most important and significant public health problems all over the world [2].
Usually, studies show that male to female ratio is 2:1. A study that included 1084 participants revealed that TBI patients have a high risk not only for post-traumatic stress disorder (PTSD) but also for other psychiatric disorders [3]. In this case, rehabilitation after a brain injury plays an important role, and it should remain a priority during hospitalization and even continue after release if needed. Mortality across all TBI severities is considered to be approximately 3%, but morbidity remains a more difficult factor to estimate [3]. In recent years, mortality decreased, possibly due to the fact that awareness has increased, guidelines have appeared and are being implemented, structuralizing management, and technological advancements in treatment regimens. It is a reality that many patients with TBI do not reach for medical care, and so the overall rates for TBI are most likely underreported [1]. The major risk factors for TBI in the US are described in Figure 1 below:
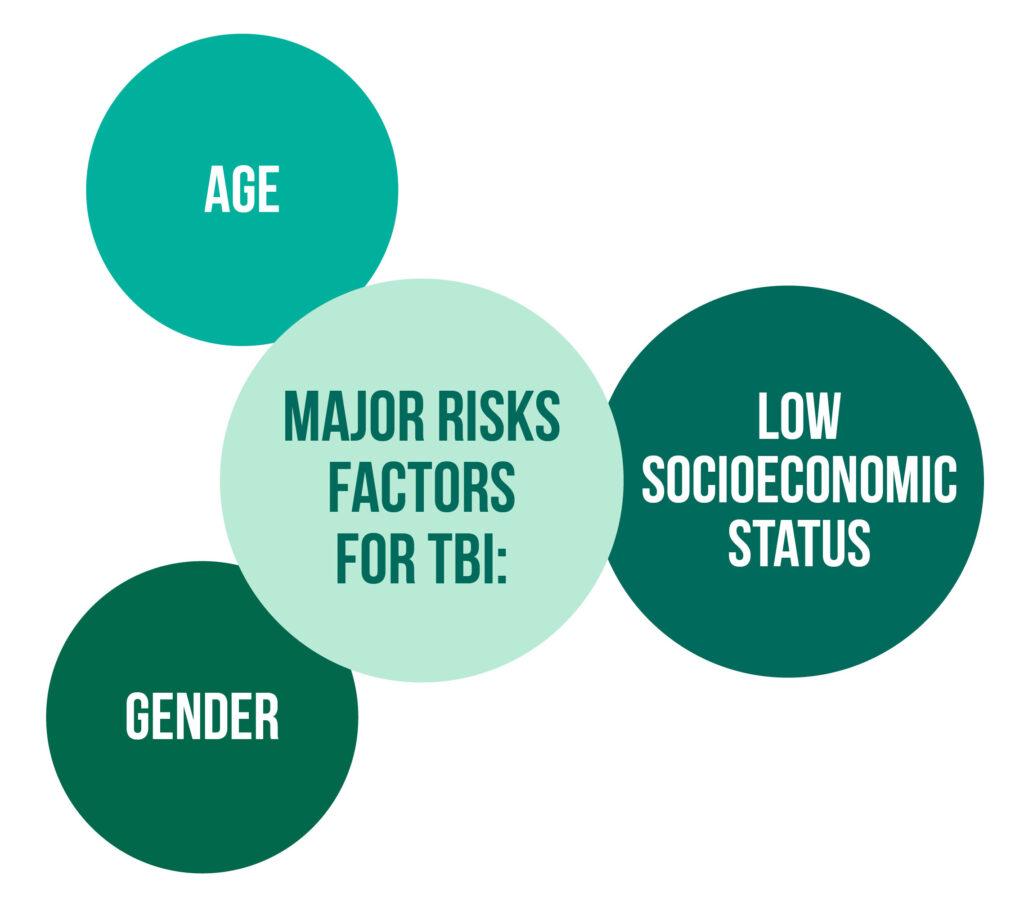
It was shown that persons at the extremes of age have the highest incidence rate. The rate among men is almost twice that of women, probably due to the fact that they tend to have more risk-taking behavior and engage in high-risk activities. In the United States, falls are the leading cause of TBI, followed close by motor-vehicle traffic accidents and assaults [2].
Fatigue frequency after TBI
Andelic et al. showed in their research that fatigue represents one of the most important subjective symptoms that patients report after suffering a brain injury. It is defined as “the awareness of a decreased capacity for mental and/or physical activity because of an imbalance in the availability, utilization, or restoration of resources needed to perform activities” [4]. The estimated post-TBI fatigue varies greatly, from 21% to 70% of patients, but is constantly higher when compared to the general population (10-20%).
Research shows that complaints of fatigue begin as soon as a few days or weeks post-TBI and seem to persist in time [5]. Over time, it was shown that the majority of patients report a decrease in self-reported fatigue, but some of them still suffer from persisting fatigue even after a long period of time since the TBI happened. Mollayeva et al. showed in their systematic review that the mean frequency of significant fatigue has a tendency to decrease from one month (47%) to one-year post-injury (37%). But we have to acknowledge that the majority of studies included patients that sustained a mild TBI. According to other studies, fatigue can remain a serious problem for patients even several years after the injury or may even worsen in time [6]. Previous research showed a decrease in fatigue after a year in patients that suffered a mild TBI, stable fatigue in those that suffered a moderate TBI, and an increase in fatigue in patients that suffered a severe TBI. In contrast, there were studies that concluded that long-lasting fatigue after a brain injury is not limited only to those that suffered a severe TBI but can also be present in patients with milder brain injuries, and also, it can be caused or exacerbated by emotional and cognitive symptoms, pain or sleep disturbances in TBI patients [6]. The majority of longitudinal studies did not find the severity of the TBI to be a predictor of the appearance in time or of the severity of fatigue. Although one might expect that patients with more severe injuries would have greater chances of fatigue appearance following the TBI, the connection between these two constructs is not as straightforward as one would expect [5].
Persistent fatigue is not only a distressing condition for patients, but it was also shown that it could be associated with a variety of different negative outcomes. Many studies show that it is contributing to the decreased quality of life and the overall disability of patients. The link between fatigue and anxiety or other psychiatric disorders, insomnia and other sleep-wake disturbances, pain, and other physical disturbances was researched in previous studies. Fatigue levels are thus probably linked to the stabilization and evolution of other TBI-related problems such as anxiety, depression, pain, sleep, and cognitive difficulties. All of these evolve in time, and patients must adapt to them, which may add to the core fatigue related to neurological injury. Only a small number of studies tried to examine the potential global impact of fatigue, such as one’s ability to return to work [5]. The interconnection that this two share can work both ways. Ponsford et al. did not find any association between fatigue and one’s ability to return to work, while Oullet, Morin, & Lavoie did remark that being on disability leave or being inactive from work (active work or volunteering) for a long period of time is associated with the presence of significantly more severe fatigue in these persons [5].
Premorbid variables might contribute additionally to vulnerability and predisposition for the development of fatigue after TBI. Among these:
- personality traits
- mental/emotional health problems
- pre-existing fatigue.
To a lesser extent, Andelic et al. showed there was an association between fatigue and personal factors such as gender, age, and education. It is essential to recognize that, after stroke, there are gender differences in the prevalence and severity of fatigue, as some studies suggest. Even so, there were inconsistent effects of age and gender after TBI, but higher education was linked to a higher level of post-TBI fatigue [3].
Despite the growing number of studies researching the link between fatigue and TBI, there is a lack of large-scale studies on longitudinal fatigue changes across both injury severity and acute clinical care pathways. The majority of studies carried out until now were conducted on patients after a mild TBI and at varying time points post-injury. Large-scale studies are essential in order to increase the knowledge concerning which factors might influence the most the persistence and occurrence of fatigue after a brain injury, as well as help in the development of preventive measures and targeted fatigue interventions [4].
Assessment of fatigue after TBI
For the assessment of different aspects of fatigue, several scales have been developed. Many of them contained a high number of questions which made it difficult and tiring for the patient to complete them, especially when other symptoms of brain injury needed to be evaluated. One of these scales is the River-mead Post-Concussion Symptoms Questionnaire (RPQ), a self-rated questionnaire that assesses the severity and presence of common post-TBI symptoms. In this questionnaire, fatigue is one of the most often affirmed symptoms, and that is why RPQ is useful in evaluating the progression or regression of symptom severity. In the factor analysis of the RPQ, fatigue was classified as either an emotional/somatic or cognitive symptom or as a somatic/physiological symptom, and it was linked to the limitation of daily functioning in patients. Because the fatigue item in the RPQ estimates very well the subjective experience of fatigue after a TBI, it was used on a sample of patients from the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) study. The aims of the study were:
- to assess the severity and frequency of fatigue at baseline, three, and six months after TBI across gender, age, patient’s clinical pathway in the acute phase, and severity of the injury
- to investigate if socio-demographic factors, pre-, and postinjury comorbidities, and injury severity characteristics can predict fatigue changes across the first six months after a TBI
The researcher’s hypothesis was that fatigue is a significant burden for most patients after TBI, regardless of the time since the injury or the injury severity.
The CENTER-TBI study, from which patients were selected, was a prospective observational longitudinal multicenter cohort study conducted in 65 participating centers from Israel and Europe. It enrolled patients with TBIs of different severity and was conducted from December 2014 until December 2017. The only exclusion criterion was the presence of pre-existing neurological disorder that could affect the outcome. The inclusion criteria were:
- clinical diagnosis for TBI
- presenting to the medical center in the first 24 hours after injury
- indication for a CT scan
- obtained consent adhering to national/local legal and ethical requirements
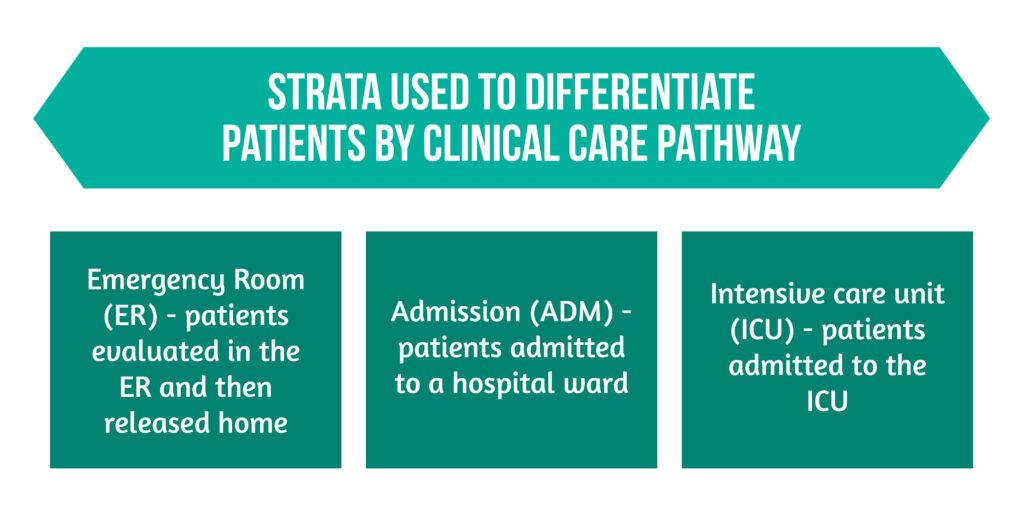
There were three strata used to differentiate patients by clinical care pathway are highlighted in Figure 2 below:
Study participants and data analysis
CENTER-TBI enrolled a total of 4509 patients. All patients who answered the question about fatigue from the RPQ at least once at baseline, 3, and 6 months after the injury were selected. As a result, 3354 patients were included in this study. From these :
- 2286 answered the RPQ-fatigue question at baseline
- 2164 answered the RPQ-fatigue question 3 months after the injury
- 2253 answered the RPQ-fatigue question 6 months after the injury
Both adults (age>16 years) and children (age<16 years) and/or their parents were asked to rank the severity of fatigue by comparing it with their preinjury status during the last 24 hours. A 5-point Likert scale was used for rating, from 0, which meant “no problem” to 4, which meant “severe problem”. The data were collected in face-to-face interviews or per electronic or postal questionnaires at baseline, 3 and 6 months follow-ups. For rating the symptoms as mild, moderate, or severe, the cut-off value used was ≥2. Also, due to the fact that in clinical practice, the group of patients rated as moderate or severe may be difficult to treat due to the impact of fatigue on daily activities, a cut-off value of ≥3 was also applied, corresponding to symptoms that were rated as severe and moderate.
Injury-related and socio-demographic characteristics that were collected during the study and used as independent variables were :
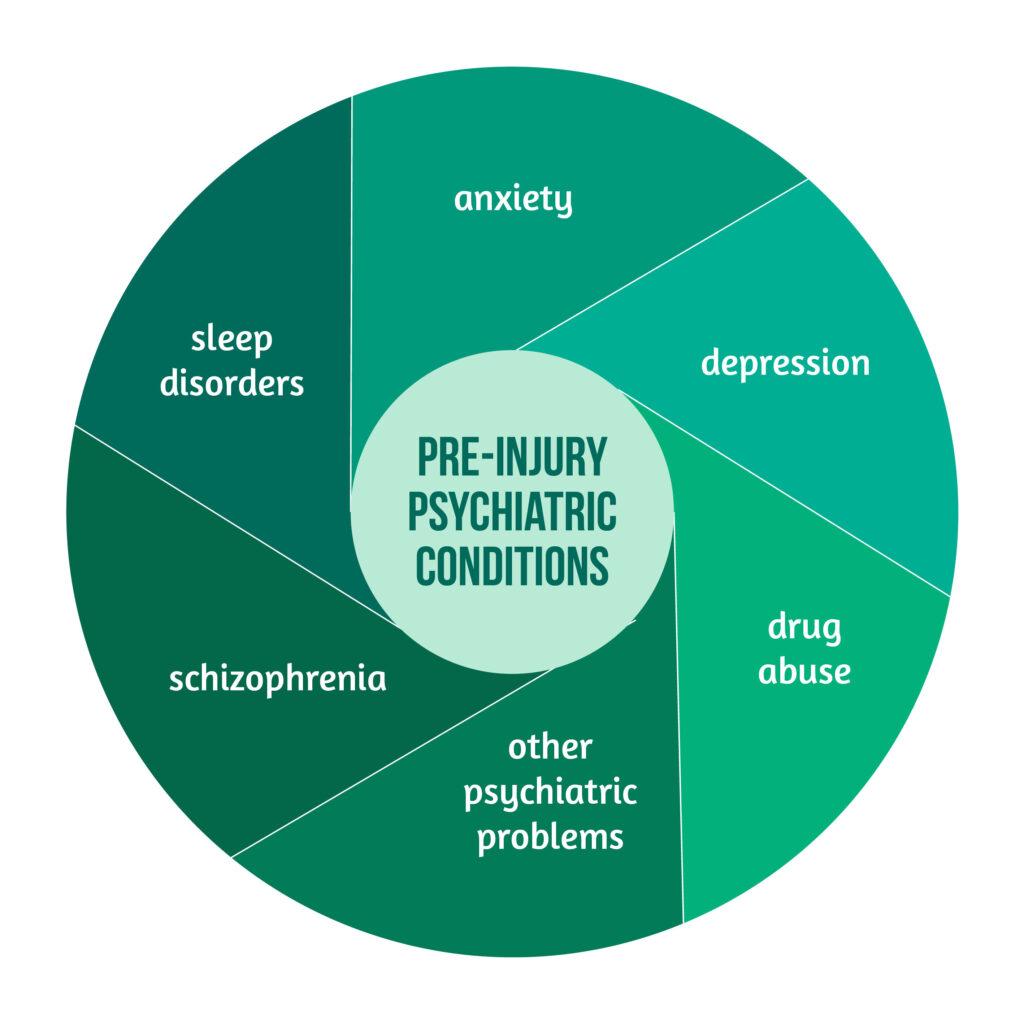
- age
- gender
- education
For the assessment of pre-injury comorbidities, the pre-injury American Society of Anesthesiologists Physical Status Classification System score (ASA-PS) was used. Pre-injury psychiatric conditions are highlighted in Figure 3, while injury-related variables that were collected are underlined in Figure 4.
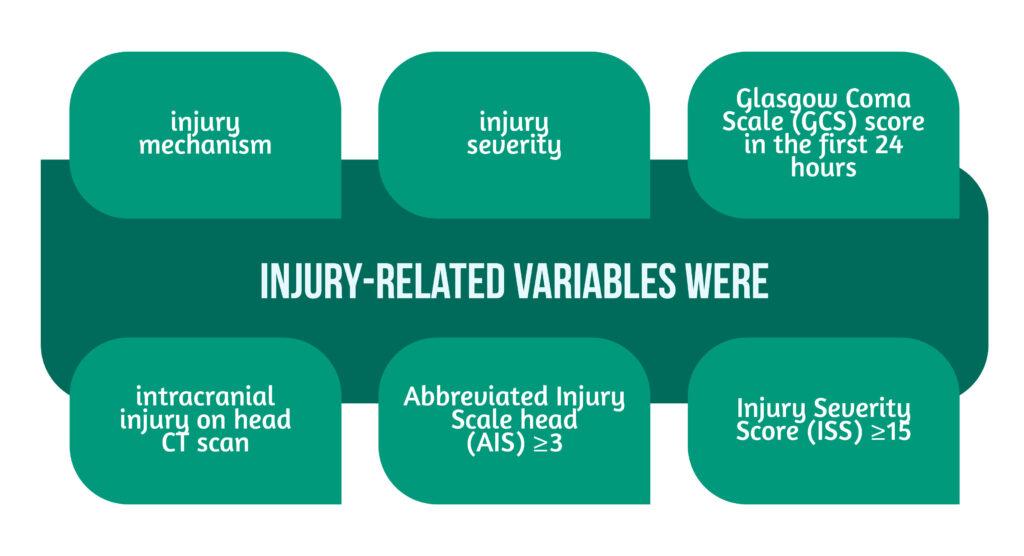
The last two points were considered to be a marker for major trauma.
In this manuscript, the CENTER-TBI dataset version 2.0 was analyzed. The frequency of patients accusing fatigue was assessed per patient strata, GCS severity level, gender, and age group.
The results showed that 808 patients were included in the ER stratum, 1351 were included in the ADM stratum, and 1195 were included in the ICU stratum. The median age was 49 years, and the majority of patients (65%) were male. The median years of education were 13 years. Of all the patients, 2286 reported the fatigue item at the baseline and, as a result, were included and evaluated in this study. Of these, about 46,9% were accused fatigue (cut-off score≥2). When the moderate/severe cut-off score was used (≥3), the frequency was halved. It was observed that the highest median fatigue score was in patients admitted to the ICU. The frequency of reported fatigue was higher in women across all age groups. From these, the highest frequency of moderate and severe fatigue was found in women aged 50-60 years and males aged 0-10 years, and the lowest in women 60-70 years and males over 70 years.
Overall, no significant statistical differences were seen in the first 6 months after the injury between patient strata. In the ER and ADM, there was a significant difference within the group due to a decrease in the fatigue score from baseline to 6 months, but this difference was not also observed in the ICU group.
Two models were used in the predictive analyses to examine whether changes in fatigue scores≥3 or ≥2 could be predicted by injury severity indicators, demographic variables, or comorbidities. The first model suggested that patients that were known with psychiatric problems had the tendency to report higher fatigue scores starting at the baseline and increasing over time. In contrast, those without a known psychiatric condition reported decreased scores over time. The second model showed that the same predictors as in model 1 were statistically significant.
Lessons on Post-TBI fatigue from the CENTER-TBI Study
The study of Andelic et al. assessed the frequency of fatigue after a TBI, changes in fatigue across clinical care pathways and severity of the injury, and the predictor factors of fatigue severity levels.
Fatigue was observed to be a widespread symptom after a TBI, with a high frequency throughout the whole sample of patients: 47% of them reported fatigue at the baseline, 48% reported fatigue at 3 months, and 46% at 6 months. The frequency was higher in the ICU patients, those who suffered a moderate or severe brain injury, and those with more severe trauma and intracranial injuries. As expected, the level of fatigue was quite stable over the 6-month post-TBI period.
A link was found between fatigue levels and demographic factors such as gender, age, and education.
The link between women, education level, and the higher frequency of reported fatigue was also described previously in other studies. Also, the research shows a relationship between severe TBI and overall trauma and fatigue. Preinjury and postinjury comorbidities also predicted fatigue levels. This is important for rehabilitation, given the impact that these pathologies have on the patient’s daily activities and quality of life.
The current study’s limitations might be the fact that these findings are not generalizable to all individuals sustaining a mild TBI without the indication for a head CT scan. Another one is the use of a single-item operationalization of fatigue.
Conclusions on tatigue frequency after TBI
Fatigue is an important symptom that can appear after TBI, and gender, education level, and previous comorbidities are just some of the factors that can influence it.
Each year, it is a well-known fact that approximately 69 million individuals suffer a TBI. More studies are needed in order to advance the clinical decision-making process and for targeted medical treatment of fatigue which appears to be an increasing problem after TBIs [3–4].
References
- Galgano M, Toshkezi G, Qiu X, Russell T et al., ‘Traumatic Brain Injury’, Cell Transplant. 2017, vol. 26, no. 7, pp. 1118–1130, doi: 10.1177/0963689717714102.
- Majdan M, Plancikova D, Brazinova A, Rusnak M et al., ‘Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis’, Lancet Public Health, vol. 1, no. 2, pp. e76–e83, 2016, doi: 10.1016/S2468-2667(16)30017-2.
- Corrigan JD, Selassie AW, & Orman JAL, ‘The epidemiology of traumatic brain injury’, J. Head Trauma Rehabil., vol. 25, no. 2, pp. 72–80, Apr. 2010, doi: 10.1097/HTR.0b013e3181ccc8b4.
- Georges A & Das JM, ‘Traumatic Brain Injury’, in StatPearls, Treasure Island (FL): StatPearls Publishing, 2022. Available: http://www.ncbi.nlm.nih.gov/books/NBK459300/
- Andelic N Røe C, Brunborg C, Zeldovich M et al., ‘Frequency of fatigue and its changes in the first 6 months after traumatic brain injury: results from the CENTER-TBI study’, J. Neurol. 2021, vol. 268, no. 1, pp. 61–73, doi: 10.1007/s00415-020-10022-2.
- Beaulieu-Bonneau S & Ouelle MC, ‘Fatigue in the first year after traumatic brain injury: course, relationship with injury severity, and correlates’, Neuropsychol. Rehabil. 2017, vol. 27, no. 7, pp. 983–1001, doi: 10.1080/09602011.2016.1162176.