Authors: Lavinia Filip, Silvina Ilut
Keywords: Traumatic brain injury, emotions, anxiety, depression
Which are the emotional changes after TBI?
Traumatic brain injury (TBI), a form of acquired brain injury, occurs when a sudden trauma causes damage to the brain. TBI can result when the head suddenly and violently hits an object or when an object pierces the skull and enters brain tissue, representing a medical, healthcare, social, and economic burden worldwide [1].
In low and middle-income countries, the incidence of TBI due to traffic incidents is increasing, while in high-income countries, TBI increasingly affects elderly people, mostly due to falls [2].
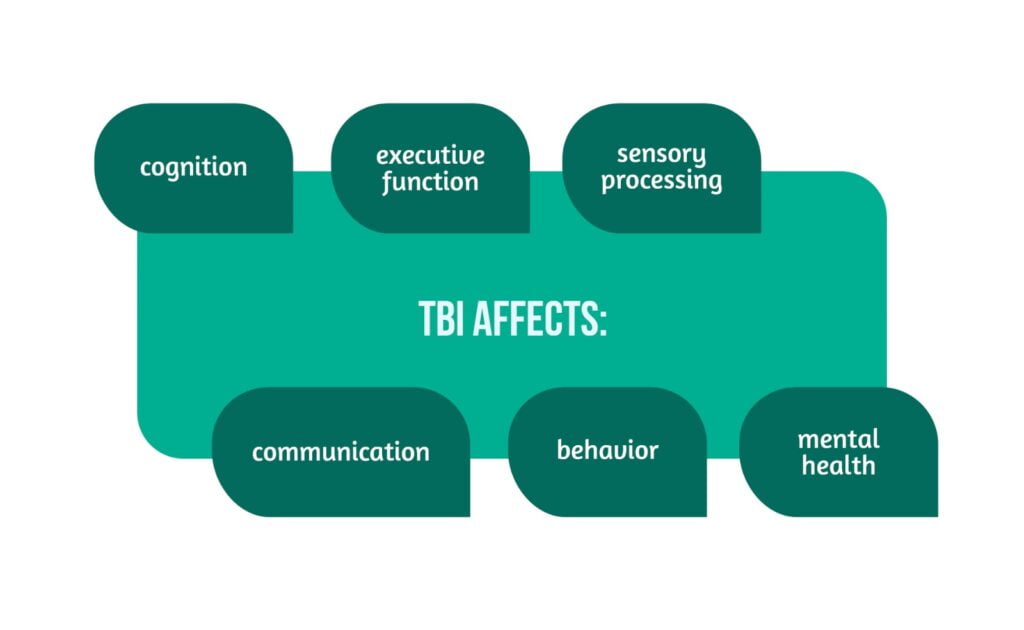
Disabilities resulting from a TBI include problems with:
- cognition (thinking, memory, judgment, and reasoning)
- executive function (problem-solving, multitasking, organization, decision-making) sensory processing (sight, hearing, touch, taste, and smell)
- communication (difficulty understanding speech or writing, difficulty speaking or writing)
- behavior or mental health (depression, anxiety, personality changes, aggression, emotional changes) [3] (Figure 1).
What are the most common regions of the brain affected by TBI?
Contusions, or focal damage to the brain’s tissue and vasculature structure, are most likely to occur in frontal and temporal regions where brain tissue is adjacent to the bony ridges and protuberances of the interior base of the skull. Intracranial hemorrhage may occur, requiring immediate medical attention. Diffuse axonal injury (DAI) refers to damage to the brain’s white matter tracts caused by sheering forces resulting from the brain rotating within the skull. Due to the axon’s viscoelastic properties, axonal damage is prevalent across levels of injury severity.
DAI is likely to be the principal pathologic substrate of long-term deficits associated with moderate TBI. Given the high prevalence of executive deficits in patients with TBI, it is not surprising that the frontal lobes and their related circuitry (subcortical white matter, basal ganglia, and thalamus) are particularly vulnerable to TBI.
In decision-making:
- The emotional components (e.g., risk adjustment and impulse control) predominantly involve subcortical structures and the interplay between frontal and subcortical systems
- The cognitive components, such as rational choice, rely heavily on the prefrontal cortex [4].
Why do people with TBI have emotional problems?
Some of the causes for post-TBI emotional changes include
- Damage to the areas of the brain that control emotions. Changes to these brain regions and the chemicals that help the brain work can affect how the person with TBI experiences or expresses emotion.
- Difficulties in coping with the injury. People with TBI may need to adjust to a loss of independence or changes to their role in their family and society. These changes can lead to frustration and dissatisfaction with their life.
- Changes in thinking abilities, such as memory, attention, speed of thinking, and reasoning. These changes can cause them to feel overwhelmed when unable to remember things or keep up with what others are doing or saying. This might elicit an emotional response of sadness, worry, or anger.
- Use of alcohol or other drugs. This can lead to emotional changes, and emotional distress may also lead to alcohol and drug use
- Medication side effects.
- Depression, anxiety – People who had problems with depression or anxiety before the TBI may find that these problems are worse after the TBI. They may feel isolated, depressed, or misunderstood, which can also affect emotions [5].
What are the most common emotional problems after a TBI?
Post-TBI anxiety has been found to manifest in various forms, such as post-traumatic stress disorder, generalized anxiety disorder, obsessive-compulsive disorder, irritability, anger, and aggression. Thus, it is relatively common for TBI to lead to the development of one or more specific anxiety disorders, and healthcare providers need to become familiar with their characteristics in this specific population.
Following TBI, depression is more common than mania. Depression occurs more frequently with lesions of the frontal and temporal lobes and left anterior lesions. The recovering patient must come to terms with physical and mental limitations and may psychologically mourn those functions impaired or lost. The common symptoms of depression may be less pronounced in TBI patients due to overall personality flattening [7, 9].
Post-traumatic stress disorder (PTSD)
PTSD is characterized by the development of symptoms resulting from direct exposure to an extreme traumatic stressor, such as:
- actual or threatened death
- serious injury
- other threat to one’s physical integrity
- witnessing an event that involves death, injury, or a threat to the physical integrity of another person.
The person re-experiences the traumatic event through intrusive symptoms (nightmares); takes great efforts to avoid reminders of the incident; experiences changes in mood and cognitive processes (changes in beliefs about the self and the world); experiences changes in arousal and physiological reactions (sleep disturbances, startle response); with symptoms persisting for more than one month following the traumatic incident [6].
Generalized Anxiety Disorder (GAD)
Generalized Anxiety Disorder (GAD) is characterized by excessive worry and/or distress about a myriad of activities (work, school, relationships) that cannot be attributed to another anxiety disorder.
The worry must be difficult to control and is accompanied by a minimum of three somatic symptoms, including the ones in Figure 2.
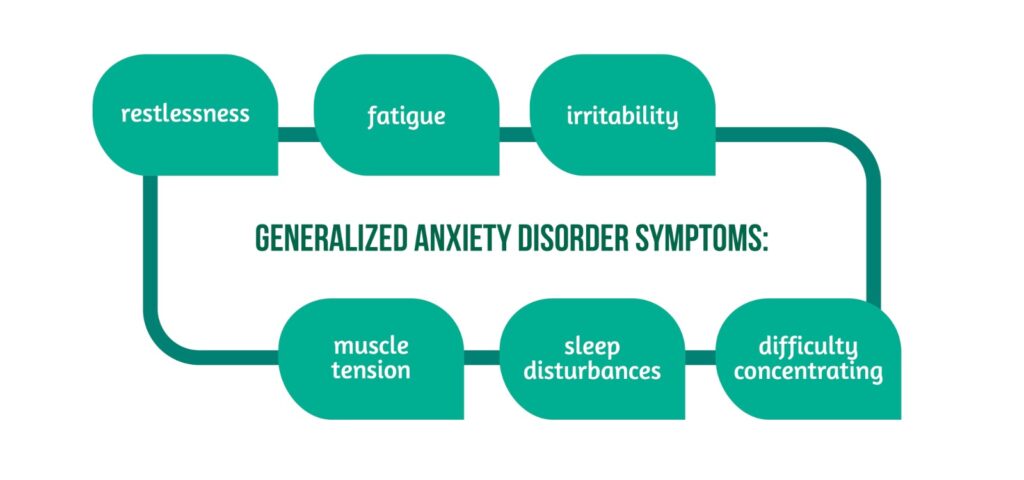
The worry and accompanying symptoms should be present for at least six months before diagnosis. In the context of TBI, it is important to note that this diagnosis cannot be made if the disturbance is attributable to the physiological effects of a medical condition. Thus, in cases where generalized anxiety appears post-injury, it is more appropriate to diagnose an Anxiety Disorder Due to a General Medical Condition. Retrospective studies that have evaluated the development of psychiatric disorders following TBI found GAD to be the most common anxiety disorder diagnosed following head injury [6].
Some suggestions for the management of anxiety include:
- exercising
- eating well
- avoiding alcohol and drugs
- sleeping well
- preventing another TBI
- medical treatment [5].
Obsessive-Compulsive Disorder (OCD)
OCD is characterized by impairing obsessions and compulsions marked by recurring persistent thoughts, beliefs, and actions. Individuals are often able to recognize their obsessions and compulsions as irrational but feel compelled to complete them anyway. However, recent changes to the diagnostic criteria for OCD now include individuals presenting with obsessive-compulsive tendencies and low to no insight into their presenting behaviors.
OCD is relatively rare in the general population, and this remains true post-TBI, with approximately 3% of TBI survivors developing OCD [6].
Depression
Depression is a feeling of sadness, loss, despair, or hopelessness that does not get better over time and is overwhelming enough to interfere with daily life.
Some symptoms of depression include the ones presented in Figure 3.
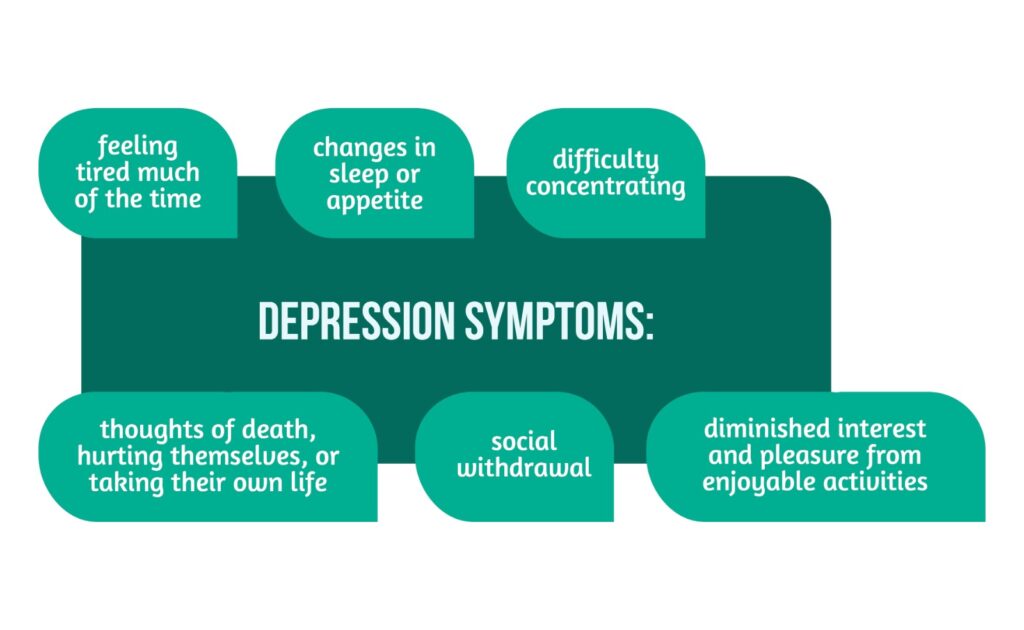
Depression is a common problem after TBI. About half of all people with TBI are affected by depression within the first year after injury. Even more (nearly two-thirds) are affected within seven years after injury. In the general population, the rate of depression is much lower, affecting fewer than one person in 10 over one year [7].
Irritability, anger, and aggression
Irritability is an emotional state in which a person has a short temper and is easily annoyed or angered. As a result, small things can lead to harsh reactions. This is most likely to happen if the person does not know how to manage their feelings or if the person is stressed.
Anger is an emotion. It’s a strong feeling of annoyance or displeasure. Sometimes angry emotions can get intense and feel out of one’s control. Anger can lead to aggressive acts. When angry, people may feel the tension in their forehead, jaw, shoulders, or fists. They may feel their heart beat faster, and their bodies may feel hot.
Aggression is a type of behavior. It is often an expression of anger. Actions can range from mildly aggressive to extremely aggressive. Aggression can be hurtful comments. It may include insults, cursing, or yelling. On the more extreme and less common end, it can include acts of violence, such as throwing things or hitting someone or something.
Irritability and anger are more common in people with TBI than they are in people without. Some research shows that up to three-fourths of people with TBI have irritability. In addition, up to 50% of people with TBI have problems with anger. A person who was not prone to irritability or anger before their TBI may now be easily irritated or angered after their TBI. Irritability and anger can be sudden and unpredictable. These feelings may be triggered more easily than before.
Anger and aggression can lead to behaviors that are difficult to control after a TBI. A TBI can make it hard for a person to talk respectfully about things that make him/her angry or frustrated. The person may also find it hard to stop an aggressive response, such as shouting, saying mean things, or cursing. Sometimes, they may express anger through physical acts, such as throwing things, punching a wall, or slamming doors. In more extreme and rare cases, anger can lead to physical fights, such as hitting others [8].
Emotional changes after TBI – what can be done?
Rehabilitation is a broad healthcare field primarily concerned with reducing patients’ disabilities and enabling their independent functioning following a disease or injury. There are many things that people who suffer a head injury and emotional problems can do:
- Get help from family members
- Psychotherapeutic (counseling) sessions and medical treatment
- Identify and avoid stress and stressful situations, which can trigger emotional distress.
- Exercise and implement a healthy diet
- Join a support group
Understanding what causes emotional problems like anxiety or depression after a TBI is important in the pursuit of finding the right treatment methods [5].
For more information about the impact of TBI visit:
- Immune response post-TBI
- How does TBI affect the functions of patients?
- Advances in TBI care and therapies
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
References
- The National Institute of Neurological Disorders and Stroke; Maryland; Brain Injury 2022. Available from: https://www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury
- Maas AIR, Menon DK, Adelson PD. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987-1048. doi:10.1016/S1474-4422(17)30371-X
- The Mayo Clinic; Minnesota; Traumatic brain injury, 2021. Available from: https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557
- Rabinowitz, AR & Levin HS. Cognitive sequelae of traumatic brain injury. The Psychiatric clinics of North America 2014, 37(1), 1–11. https://doi.org/10.1016/j.psc.2013.11.004
- Changes in Emotion After Traumatic Brain Injury. Model Systems Knowledge Translation Center (MSKTC). Retrieved from: https://msktc.org/tbi/factsheets/changes-emotion-after-traumatic-brain-injury
- Mallya S, Sutherland J, Pongracic S, Mainland B, & Ornstein TJ. The manifestation of anxiety disorders after traumatic brain injury: a review. Journal of neurotrauma 2015, 32(7), 411–421. https://doi.org/10.1089/neu.2014.3504
- Depression After Traumatic Brain Injury. Model Systems Knowledge Translation Center (MSKTC). Retrieved from: https://msktc.org/tbi/factsheets/depression-after-traumatic-brain-injury
- Neumann D, Miles SR, Sander A, Greenwald B, in collaboration with the Model Systems Knowledge Translation Center (2021). Irritability, Anger, and Aggression After TBI. https://msktc.org/sites/default/files/MSKTC-IrrAftTBI-Factsheet-508.pdf
- Sudarsanan S, Chaudhary S, Pawar AA, & Srivastava K. Psychiatric Effects of Traumatic Brain Injury. Medical journal, Armed Forces India 2007, 63(3), 259–263. https://doi.org/10.1016/S0377-1237(07)80150-X




