Keywords: disorders of consciousness and neurorehabilitation, coma, traumatic brain injury, Glasgow outcome scale,DOC
Disorder of consciousness after TBI – why is the neurorehabilitation so important?
Disorders of consciousness are associated with severe traumatic brain injury (TBI), with most patients experiencing coma during the recovery period through stages of vegetative state or minimally conscious state and acute confusional state. A portion of patients might remain in one of these conditions permanently. Disorders of consciousness can be accompanied by other important disabilities (motor, sensory, cognitive, psychiatric, etc.) that further complicate patients’ recovery process and outcomes. Neurorehabilitation for these patients is essential for improving patient outcomes, including mortality, functional recovery, and restoration of consciousness. The level of consciousness and time post-TBI have an essential predictive value [1].
Informing the patient and their family about recovery is a fundamental pillar of neurorehabilitation. To predict this course, several factors can be considered:
- Initial physical disturbance
- Initial cognitive disturbance
- Imagery
- Glasgow Outcome Scale-Extended (GOS-E)
- Demographics
- Timely recovery
- Length of posttraumatic amnesia (PTA)
- Time to comply with commands
- Glasgow Coma Scale (GCS)
- Glasgow Outcome Scale (GOS)
- Disability Rating Scale (DRS)
- Functional Independence Measure (FIM)
- Age at the time of injury
- Duration of coma [2, 3].
Furthermore, an essential step for neurorehabilitation is the collaboration among the neurorehabilitation team, the patient, and their family. Several important aspects need to be addressed:
- The current situation of the patient
- The management of expectations regarding rehabilitation
- The stages of recovery with assistance for the transition between them
- Clarification and description of the recovery process [2, 3].
Why is neurorehabilitation needed?
The primary role of rehabilitation is to enhance physical integrity and well-being, reduce complications, and promote and facilitate natural healing. According to the patient’s needs, injury severity and type, and recovery speed, a large variety of rehabilitation strategies are used (Figure 1) [2–4].
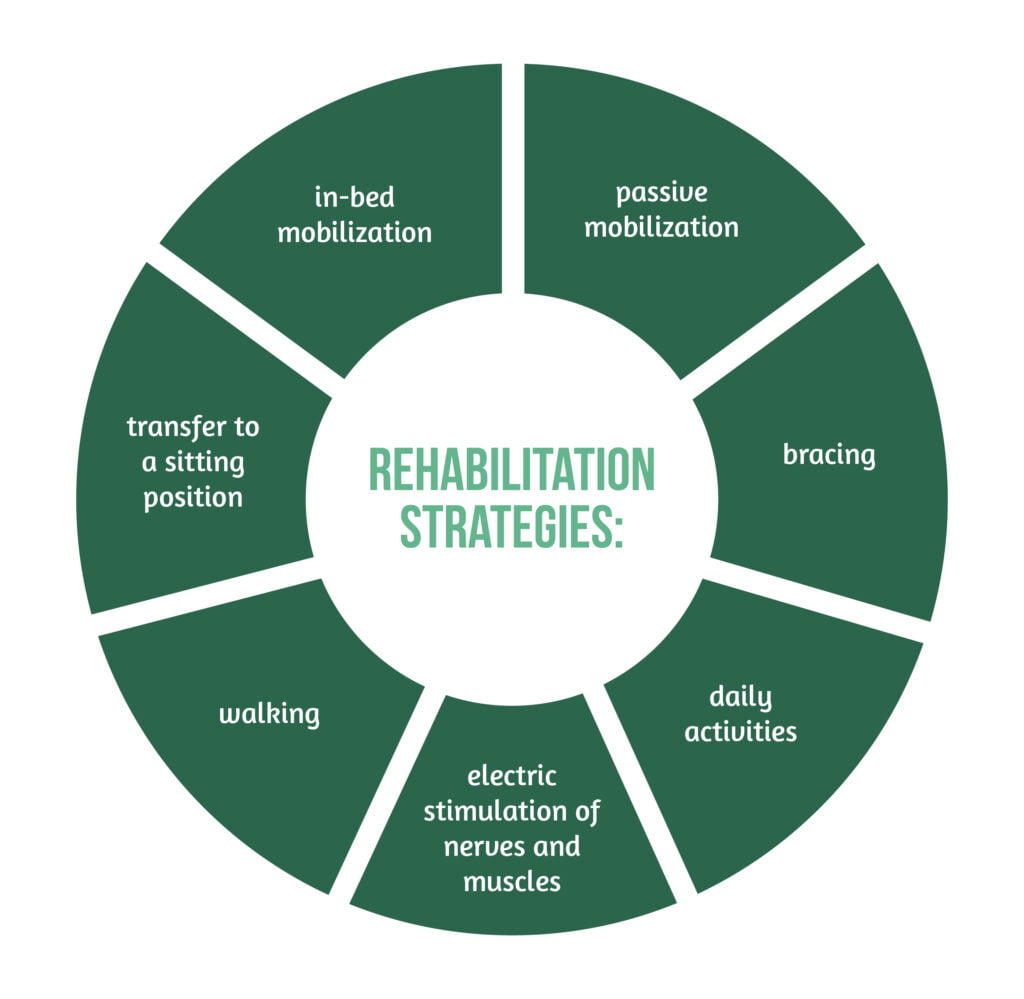
All these significantly impact the outcome of patients by reducing the overall length of stay in the hospital and the intensive care unit and improving the ability to walk and autonomy.
An essential aspect of early rehabilitation is careful monitoring by the rehabilitation team, whose neurorehabilitative decisions are made according to the patient’s state, balancing the associated risks and benefits. Early rehabilitation is contraindicated in some conditions (e.g., raised intracranial pressure) [2–4].
What types of neurorehabilitation can be done in patients with DOC post-TBI?
Ideally, the aim is to recover the ability to communicate and independently care for oneself. The neurorehabilitation team must consider all factors that might interrupt rehabilitative care, slow the rehabilitative process, limit the patient’s physical abilities, and decide on adequate treatment. Some of these factors are:
- pre-existing pathologies (diabetes, psychiatric disorders)
- injuries suffered concomitantly to the TBI (bone fractures, organ lacerations, etc.)
- disorders secondary to TBI (seizures, modifications in muscle tone, etc.)
- treatments for any of the pathologies mentioned above [1, 4, 6].
The neurorehabilitation team incorporates physicians, speech therapists, occupational therapists, rehabilitation nurses, neuropsychologists, physical therapists, and social workers (Figure 2). Each team member is essential for the patient’s recovery [6].

During rehabilitation, pharmacologic and non-pharmacologic therapies are used. The non-pharmacologic interventions consist of invasive and non-invasive measures. The medical management of the case and the multidisciplinary rehabilitation process, combined ideally with a minimum of 90 minutes of therapy, might improve (physical and consciousness levels). Besides the types of therapy mentioned above, sensory stimulation may help increase the responsiveness of patients. The stimulation can be done with photos of family or friends, a known movie, playing music, talking, spraying a known perfume, or simply touching [6, 7].
Another essential aspect of neurorehabilitation is the systematic assessment of the patient’s evolution and treatment modification by the state to provide optimal care [1, 4, 6].
Should the rehabilitation process be started early, during a hospital stay?
Rehabilitation after TBI starts in an early stage and has significant benefits for patients. The aim of early rehabilitation resides in the improvement of the patient’s prognosis and the reduction of several complications:
- Muscle contractures due to immobility
- Bladder and bowel dysfunction
- Skin lesions
- Sleep disturbances [2–4, 8].
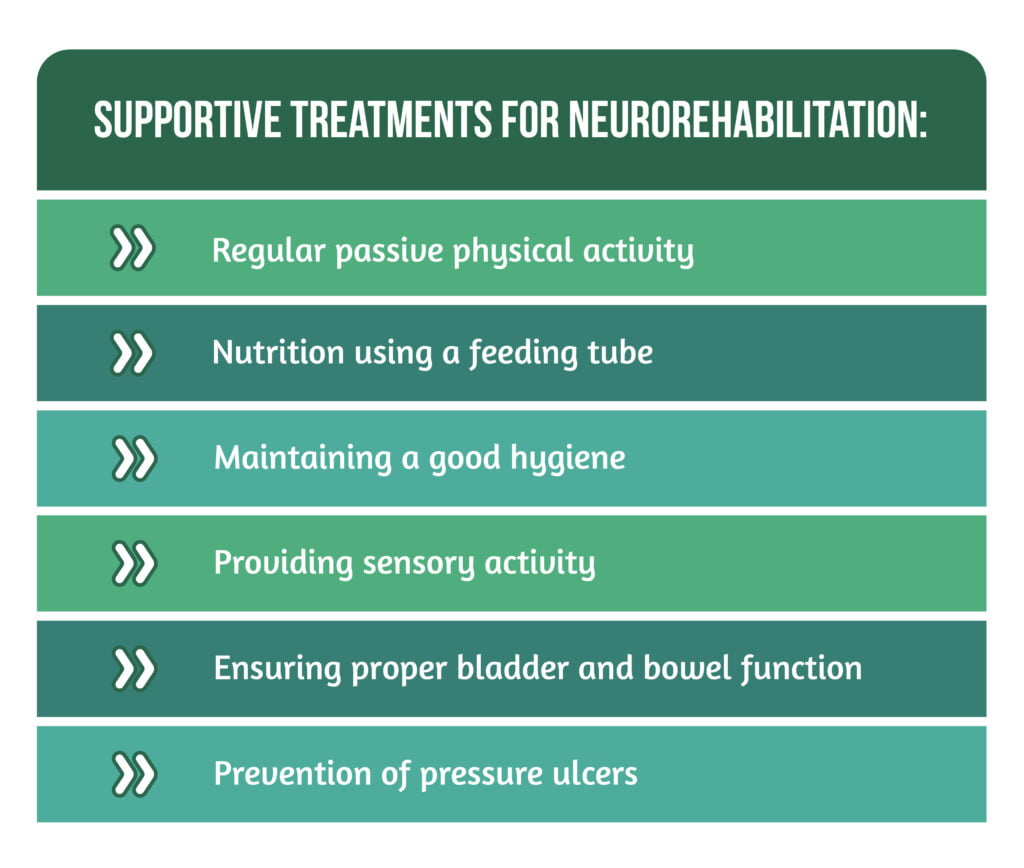
Additionally, the supportive treatment adds to facilitating the natural improvement post-TBI (Figure 3) [7].
What is the time of the recovery process?
Overall, the evolution of the recovery process is inconsistent, with periods of amelioration and degradation, this characteristic representing no reason for uneasiness [2–4, 8].
The length and rate of the recovery process are variable, by the severity of the lesions, patient’s particularities, and encountered complications (spasticity, behavioral disturbances – aggression, agitation, sleep disorder, restlessness, infections-mostly urinary and pulmonary, etc.). The mechanisms leading to this variability regarding the recovery in post-TBI patients are yet to be discovered. Nevertheless, the rehabilitation process specifically addresses the patient’s needs. Some patients might have a speedy full recovery, while others might have a partial, slow recovery.
A pillar for recovery is supporting brain health (engaging in physical activity, healthy eating, and avoidance of toxins-including alcohol and other drugs) associated with neurorehabilitative measures. Most improvement is seen during the first 6 months post-TBI, followed by a slowed recovery [2–4].
What are the main takeaways regarding DOC and rehabilitation after TBI?
- TBI is a heterogenous disease leading to heterogenous disabilities by severity.
- The early rehabilitation process starts post-TBI and varies from patient to patient by the needs and patient’s state.
- Some patients might need long-term care.
- DOC can appear post-TBI, and neurorehabilitation can be implemented in these circumstances.
- Informing the patient and their family about the individual recovery process of patients and prognosis is a fundamental pillar for neurorehabilitation.
- Neurorehabilitation is a multidisciplinary field.
- The prognosis and outcomes of patients with DOC post-TBI can be improved by neurorehabilitation [2–4, 6–8].
For more information about the impact of TBI visit:
- Immune response post-TBI
- How does TBI affect the functions of patients?
- Advances in TBI care and therapies
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
Bibliography
- Giacino JT, Katz DI, Whyte J. Neurorehabilitation in disorders of consciousness. Semin Neurol. 2013;33(2):142-156. doi:10.1055/s-0033-1348960
- Iaccarino MA, Bhatnagar S, Zafonte R. Rehabilitation after traumatic brain injury. Handb Clin Neurol. 2015; 127:411-422. doi:10.1016/B978-0-444-52892-6.00026-X
- Novack T, Bushnik T. University of Washington Model Systems Knowledge Translation Center, University of Alabama TBIMS, et al. Understanding Traumatic Brain Injury Part 3: The Recovery Process, Model Systems Knowledge Translation Center, 2019; Available from: https://msktc.org/tbi/factsheets/understanding-tbi-part-3-recovery-process
- Giacino JT, Fins JJ, Laureys S, Schiff ND. Disorders of consciousness after acquired brain injury: the state of the science. Nat Rev Neurol. 2014;10(2):99-114. doi:10.1038/nrneurol.2013.279
- Raspopova M. Unnamed image. 2022 Mar 30; In: Unsplash.com; c2022; Available from: https://unsplash.com/photos/O29FNlHuKk8
- Eapen BC, Georgekutty J, Subbarao B, Bavishi S, Cifu DX. Disorders of Consciousness. Phys Med Rehabil Clin N Am. 2017;28(2):245-258. doi:10.1016/j.pmr.2016.12.003
- National Health Service. C2022. Overview Disorders of consciousness; 2022 May27; Available from: https://www.nhs.uk/conditions/disorders-of-consciousness/
- Kowalski RG, Hammond FM, Weintraub AH, Nakase-Richardson R et al. Recovery of Consciousness and Functional Outcome in Moderate and Severe Traumatic Brain Injury. JAMA Neurol. 2021;78(5):548-557. doi:10.1001/jamaneurol.2021.0084




