Keywords: TBI and taste, TBI and smell, TBI, TBI disability, olfaction, anosmia, trauma
Can TBI affect the taste and smell?
The wide variety of disabilities after traumatic brain injury (TBI) can be emotional, cognitive, behavioral, and physical, ranging from trouble with walking, feeling disorders, balance issues, or problems with sight (Figure 1). Their heterogeneity extends in accordance with the severity, type, and time passed since the injury. Two essential sequelae commonly encountered after TBI are trouble with smell and taste [1,2].

Smell and taste are of critical importance in day-to-day lives by influencing the:
- Perception of food (the ability to smell certain things like coffee, oranges, flowers, or perfume, as well as the simple types of taste: salty, sour, sweet, and bitter) – misperception of taste and smell can lead to improper use of different ingredients or improper use of a variety of foods (e.g., salt). In addition, the taste of foods may be altered (e.g., meat).
- Production of saliva – impaired smell may cause a reduction in saliva production, leading to difficulties in eating solid foods.
- Safety – inability to identify dangerous situations: rotten food or smells that would typically enable the identification of dangerous substances (e.g., the organic sulfur compounds added to methane by gas companies for the identification of dangerous leaks) and identification of different poisons or toxins.
- Perception – smell influences the perception of hygiene (by identifying unpleasant odors); it significantly influences appetite, with the loss of smell possibly leading to an increase or decrease in appetite. This can happen due to the lack of pleasure that a person usually gets from different foods, leading to a diminished interest in food and, thus, a decreased appetite and unusual eating habits. Additionally, both senses trigger the systems involved in digestion.
- Memories – smell and taste accompany different memories (e.g., the smell of cinnamon and apple might be associated with Christmas time, or the smell of Chlorine can suggest the thought of swimming in a pool) [2–4]. ‘
Why can TBI lead to loss of smell and changes in taste?
When we inhale, various scents are dissolved in the nasal mucus in the upper part of the nasal cavities. From there, the fine fibers of the olfactory nerve pass through the cribriform plate, similar to going through the wholes of a sieve, and continue their path through various other structures inside the brain up to the central part of the olfactory pathway, the temporal lobe, where the information of smell is centralized and transformed into a sensation [2,3].
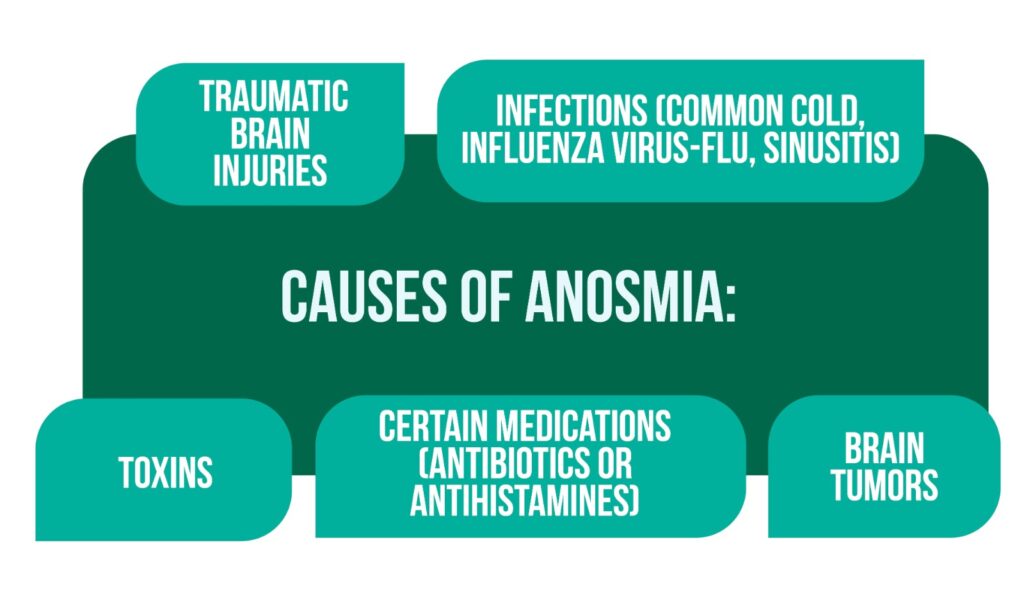
A lesion affecting the olfactory pathway can lead to anosmia (loss of smell). Infections (common cold, influenza virus-flu, sinusitis), toxins, several medications (antibiotics or antihistamines), or brain tumors can also impair the sense of smell (Figure 2) [1–3,5].
Notably, the systems responsible for taste and smell are strongly interconnected, with the responsible nerves partially overlapping. This is one of the reasons why a person who loses smell can also lose the ability to taste. Moreover, “flavor” refers to a combination of the two senses and the existing memories regarding these. Damage to one of the contributors to flavor will lead to diminished taste [3].
Can TBI follow bicycle riding lead to loss of smell? A case analysis.
Colin was on his way to school when he was knocked off his scooter, fell on the posterior part of his head, and lost consciousness for a short period. Afterward, he was alert and oriented, accusing a slight sensitivity at the place of his injury. The examination from the hospital revealed a fracture involving the base of the skull, including the cribriform plate (bone). The outcome was that:
- Colin lost his ability to smell (anosmia) due to lesions to the olfactory nerve fibers while going through the cribriform plate when the fracture occurred [2].
- Colin suffered changes in his tasting ability secondary to the loss of smell due to the connections between the two pathways [2,3].
How can problems with smell and taste be identified?
Usually, TBI patients observe changes in smell and taste while returning to previous activities. More often, the disability is identified in relation to food. They may be unable to smell various food and beverages, and the taste might also be absent or diminished (especially the flavor). An example of loss of smell and taste leading to a viral infection is when someone has a cold and a congested nose. People often realize that besides the loss of smell, they cannot feel the taste of food [2].
Who might identify and treat these types of disabilities?
A variety of medical specialists can assess these dysfunctions, including:
- Neurologists
- ENTs (ear, nose, and throat physicians) (Figure 3)
- Physiatrists
- Rehabilitation physicians.
In case of any changes in smell or taste a physician should be contacted [2].

What happens in case of loss of smell or taste, and what are some mediating strategies?
Fortunately, recovery is possible, with the chance and level depending on the severity and cause of the disability. Around one-third of TBI patients have a spontaneous, natural recovery. The shorter the period of improvement after the TBI is, the quicker and better rehabilitation is. Usually, most people encounter a boost in their senses after 6 months up to a year [2].
In the case of the impairment of smell and taste, the TBI patients and the people around them can:
- Install smoke and gas detectors
- Use fresh foods or a data labeling system (e.g., on cleaning supplies)
- Organize meals together with family and friends
- Create a daily routine by planning the meals and eating at the same hours
- Use spices and foods that represent the four main types of taste: salty, sour, bitter, sweet
- Try new recipes
- Supplement with vitamins (provided by a physician) [2,6].
Except for the loss of taste and smell what other disabilities are encountered post-TBI?
Because of the heterogeneity of TBI, loss of taste and smell are often not the only type of post-injury disability. Depending on the affected region of the brain and the severity of TBI, several other disabilities might often appear, such as problems with mobility, balance, sensitivity, and coordination, as well as psychosocial disabilities, encompassing disturbances with mood, behavior, and cognitive dysfunction. All these disabilities reflect on the social functioning and quality of life of TBI patients (social relationships, need for care, employment status, etc.) [2,7].
For more information about the impact of TBI visit:
- TBI impact on relationships
- The importance of prehospital care for severe TBI
- Mild TBI outcomes – lesssons from the CENTER-TBI study
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
References
- Schofield PW, Moore TM, Gardner A. Traumatic brain injury and olfaction: a systematic review. Front Neurol. 2014. doi:10.3389/fneur.2014.00005
- Greenwald BD, Neumann D, Dubiel R. Model Systems Knowledge Translation Center, Loss of Smell or Taste After Traumatic Brain Injury, Model Systems Knowledge Translation Center, 2019. Available from: https://msktc.org/sites/default/files/Loss-Smell-Taste-TBI-508.pdf
- Pauwels LW, Stewart PA, Akesson EJ, Spacey SD. Cranial Nerves: Function & Dysfunction, 3rd ed; PMPH USA 2010. Available from: https://books.google.ro/books/about/Cranial_Nerves.html?id=fcFxAwAAQBAJ&redir_esc=y
- Wisconsin Department of Health Services, c: 2022. Methane, 2022; Available from: https://www.dhs.wisconsin.gov/chemical/methane.htm#:~:text=Methane%20can%20form%20an%20explosive,too%20high%20to%20be%20safe.
- Cleveland Clinic, c: 2022. Anosmia (Loss of Sense of Smell) 2021; Available from: https://my.clevelandclinic.org/health/diseases/21859-anosmia-loss-of-sense-of-smell
- Headway the brain injury association, c:2022. 5 Ways to cope with taste and smell problems after brain injury, 2018; Available from: https://www.headway.org.uk/media/2805/loss-of-taste-and-smell-factsheet.pdf
- Humphreys I, Wood RL, Phillips CJ, Macey S. The costs of traumatic brain injury: a literature review. Clinicoecon Outcomes Res. 2013. doi:10.2147/CEOR.S44625




