Keywords: TBI, balance, risk of TBI, falls and TBI, balance disorders
Focus keyword: balance
How does balance work, and why do we need it?
Can TBI affect balance? The balance represents the ability of the human being to center the body on its basis of support. The type of support differs by the person’s position, allowing them to adopt and maintain various postures. For example, when in a standing position, support will be provided for the legs. Comparatively, when sitting, the support will be in the behind, thighs, and legs. Moreover, it bears importance for various everyday activities, from the simple act of standing, walking, or moving gracefully to more complex activities like self-care tasks (bathing, using the toilet, dressing) or other daily-living tasks (driving, playing sports, or working). Lastly, balance keeps people from falling [1,2].
Find more about the global incidence of TBI and the picture of TBI epidemiology in Europe over time.
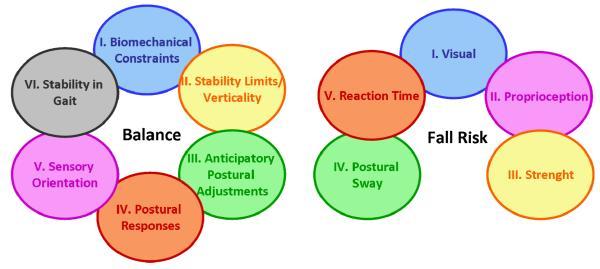
Balance is a complex ability, so it depends on the normal function of several mechanisms. For example, the ability to make postural changes to avoid falling when losing balance (or making a step back) is the result of a complex mechanism involving several systems (e.g., sensory, musculoskeletal, nervous) [1].
Consequently, any lesion to any parts of the system involved in keeping the balance will lead to decreased ability of all activities involving balance and possibly lead to TBI [1–3].
Balance is influenced by the following factors:
- muscle strength
- different senses, like a healthy inner ear for the vestibular sense or visual acuity
- coordination
- intact mental abilities [1].
As mentioned before, for balance to be maintained and for people to realize the position of their body or body parts in relation to the surroundings, environment, and gravity, several parts of the human body are used. Information on body position is provided by the eyes, ears, muscles, and joints (Figure 1).

Once the information is received, responses are executed as movements to ensure continuous body adaptation, thus maintaining balance [2]. This information helps achieve the following:
- approximating the distances of different objects from the body
- having a stable visual acuity during movement
- being able to identify changes in movements (acceleration or deceleration)
- making a postural movement as an adaptation for balance maintenance [2].
It is essential to mention that the involved mechanisms become less efficient with age, thus increasing the frequency of falls [2].
The most encountered neurological symptoms in patients with TBI:
- Dizziness
- Disorders of balance
- Fatigue
- Headaches
- Backpain
What are the consequences of falls on TBI?
The consequences of falls range in severity from the most insignificant ones to severe, even life-threatening injuries with a secondary disability or even death. The cause is the trauma that comes secondary to the fall [4]. The most affected age groups are the elderly and children. The severity of the disorder of balance varies in accordance with the amount and severity of trauma (for example suffering from a traumatic brain and spine injury and a broken leg will lead to a severe disorder of balance) and the localization and severity of the traumatic brain injury. It is essential to mention that certain medications can affect balance [1].
Traumatic brain injury is one of the main consequences of falls. Suffering a TBI can frequently lead to problems with balance and consequently to other TBIs [1]. In people suffering from mild TBI, dizziness represents the most often encountered complication after the secondary headache and pain in the neck region [3].
Noteworthy is the difference between dizziness, vertigo, trouble with balance, and lightheadedness. Frequently, the patients cannot clearly define what they are feeling, so they might say they suffer from dizziness while referring to vertigo, disequilibrium, lightheadedness, or presyncope (or almost fainting) [1,2], as showcased in Figure 2.

What causes balance disorders after TBI?
Balance disorders have several causes, mirroring the lack of information from the different processes involved.
These range from issues with:
- vision
- inner ear
- proprioceptive sensibility (the system involved in keeping the balance, especially with the eyes closed)
- injury to some parts of the nervous system (mainly the brainstem and cerebellum)
- several medications (antibiotics, blood pressure medicine, antiepileptic drugs).
Finally, having postural hypotension (lowering of the blood pressure when standing up too quickly, leading to dizziness) or trouble with mental health can also influence the risk of falling [1].
How are balance disorders diagnosed? Who gives the diagnosis?
Because of the multiple systems involved in maintaining the balance, several types of medical specialties can assess and treat balance disorders in accordance with the cause and localization of the lesion.
Consequently, balance disorders might be diagnosed and treated by a multidisciplinary team, as seen in Figure 3 below:

Currently, several tests are available for the assessment of balance, identification of abnormalities and risk of suffering from falls, and following the evolution of the symptoms [1]. The complexity of the system controlling balance has led to the need for a systematic clinical assessment of this disorder through adapted tests, thus allowing a comprehensive diagnosis and treatment. On the one hand, functional tests assess balance status overall and its response to motor tasks.
Some examples of functional tests are:
- Activities-Specific Balance Confidence Scale
- Berg Functional Balance Scale
- Balance Evaluation Systems
- Test (BESTest)
- “Up and go test”
On the other hand, the systems test assesses the balance disorder by covering the underlying cause, referring to the involved systems, some of which are:
- the BESTest
- the physiological balance profile (PPA)
- Lord`s physiological profile [5] (Figure 4).
What can be done about balance disorders?
Medical doctors will indicate the best-suited treatment for balance disorders while accounting for the cause [1].
The treatments are mainly based on different exercises to improve balance, including:
- exercises to improve the ability to:
- stand
- walk
- change postures
- change positions
- exercises to improve strength and flexibility.
Furthermore, several programs address balance disorders that are specially designed and based on the existing medical evidence [1]. One important aspect of these programs is the underlying cause of the balance disorder, thus, some of the interventions are simple maneuvers that can be done by the physician, like the Epley maneuver, which involves moving the patient in different positions to correct the imbalance at the level of the affected ear.
Furthermore, several exercises to improve balance can be done at home by the patient, while others assume medication, changes in diet, quitting smoking, and vestibular rehabilitation in patients that do not have a complete resolution of the disorder [6].
Unfortunately, the severity of the injury and patients’ comorbidities significantly impact the recovery time. For example, some people might be unable to walk (e.g., patients with balance disorder secondary to ischemic stroke) [7], while others might be unable to do rapid posture changes (e.g., patients with Parkinson’s disease) [8]. That is why the recovery time ranges from a single medical consultation to years [1].
What is the take-home message?
Balance is influenced by multiple factors, including neurological, optical, and muscular. On the one hand, balance issues are a frequent cause of falls, which leads to TBI. On the other hand, TBI can cause balance problems itself, leading to a higher incidence of balance issues in TBI patients. Diagnosing the causes of balance disorders includes multiple disciplines (e.g., neurology, otorhinolaryngology) due to the extensive number of factors involved. Consequently, the treatment will be determined based on the cause. Most often, physical exercises are recommended, which will have to be followed, in some cases, for multiple years before the patient recovers [1–3].
References
- Model Systems Knowledge Translation Center (MSKTC), Balance after Traumatic Brain Injury, January 2021, Available from: www.msktc.org/tbi/factsheets , accessed on 08.05.2022
- Brandt T, Dietrich M, Strupp M. Vertigo and Dizziness, 2nd ed, cSpringer-Verlag London 2013, , pg. 1, 145-151, DOI https://doi.org/10.1007/978-0-85729-591-0
- Ropper AH, Samuels MA, Klein J, Prasad S. Adams And Victor`s Principles Of Neurology 11th ed, cMcGrawHill 2019, pg. 313-316. Available at: https://accessmedicine.mhmedical.com/book.aspx?bookID=1477
- Centers for Disease Control and Prevention. Alexis B. Peterson, Scott R. Kegler, Deaths from Fall-Related Traumatic Brain Injury — United States, 2008–2017, March 6, 2020 / 69(9);225–230, available at https://www.cdc.gov/mmwr/volumes/69/wr/mm6909a2.htm#:~:text=Among%20all%20age%20groups%2C%20falls,disruption%20of%20normal%20brain%20function
- Mancini M & Horak FB. The relevance of clinical balance assessment tools to differentiate balance deficits; 2010; European journal of physical and rehabilitation medicine, 46(2), 239–248. Available at: https://pubmed.ncbi.nlm.nih.gov/20485226/
- National Institute on Deafness and Other Communication Disorders, Balance Disorders, 2018; Available from: https://www.nidcd.nih.gov/health/balance-disorders#g
- Arienti C, Lazzarini SG, Pollock A, Negrini S. Rehabilitation interventions for improving balance following stroke: An overview of systematic reviews. PLoS One. 2019;14(7):e0219781. doi:10.1371/journal.pone.0219781
- Park, J. H., Kang, Y. J., & Horak, F. B. What Is Wrong with Balance in Parkinson’s Disease?. Journal of movement disorders 2015, 8(3), 109–114. https://doi.org/10.14802/jmd.15018




