Keywords: TBI, fuel, treatment, glucose
Introduction | Brain injuries and mental illness
Traumatic brain injuries (TBI) and their consequences remain an intensively studied but little-known subject. The effects of brain trauma differ from one patient to another and change over time. Some patients have complications of a TBI that affect their quality of life, while in others, the healing is complete [1].
It is essential to know how the human brain works to ensure the treatment of concussions, brain injury, and mental illness (CBIMI). Unfortunately, despite the increased interest and research on mental health and TBI, these conditions are still misdiagnosed and inadequately treated [1].
How does the brain function?
Concussions are a mild form of TBI that does not involve loss of consciousness or its loss for a brief period [2]. Several animal studies were carried out to better understand the brain changes and mental illnesses that occur after a TBI but with no definitive conclusions on identifying the causes of depression or post-concussion syndrome.
For the proper development of the processes at the brain level, such as blood supply, oxygen supply, and the functioning of neurotransmitters, an adequate level of fuel is needed [1]:
- Glucose is the primary fuel used by the brain when it is available. The brain uses between 20 and 40% of the total glucose in the body, being the most significant consumer [1]. Glucose:
- Has a vital role in cellular respiration, which is dependent on its presence
- Is used as fuel in the brain and the rest of the body.
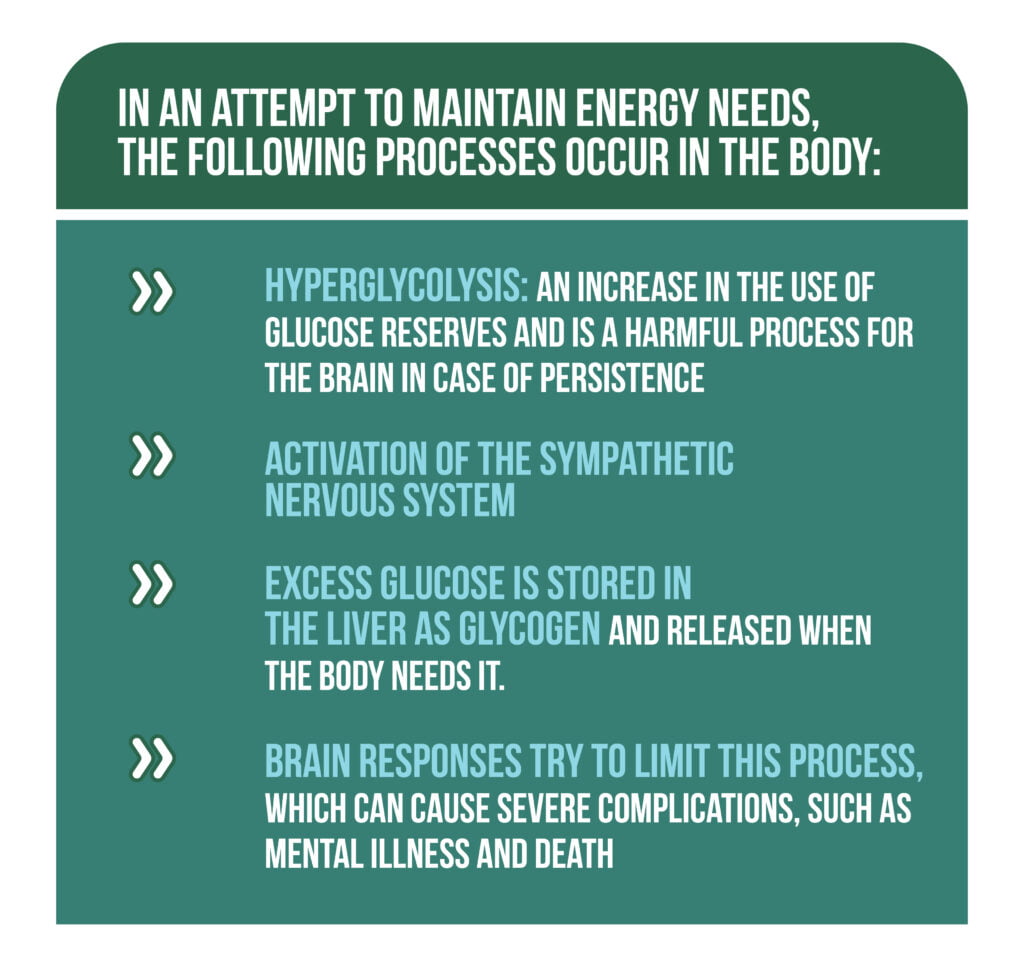
- Excess is stored in the liver as glycogen and released when needed.
- The brain stem is the first to receive it because it supports essential body functions such as breathing and heart pumping.
- Secondly, it is allocated to the cerebral cortex, which is responsible for higher functions (e.g., vision, language, and thinking).
- Ketones are the secondary fuel used in case of a lack of glucose in crisis, such as intense physical exercise, starvation, or in patients with diabetes [1].
What is the mechanism of cerebral dysfunction?
TBI causes the following changes at the brain level:
- Activation of the sympathetic nervous system, with a role in the “fight or flight” responses, determines a limitation of the amount of fuel distributed.
- In conditions of fear and trauma, the brain needs more fuel to maintain vital functions (Figure 1) [1].
What are the consequences of the lack of fuel at the cerebral level?
After a TBI, due to the limitation of the amount of brain fuel, symptoms of CBIMI may appear. In the case of a first mild trauma, patients may present mild and short-term symptoms (brain or mental). However, sometimes, some TBIs remain undiagnosed due to the absence of symptoms.
In patients with severe TBI, permanent brain disorders may appear from the first traumatic event. Every brain injury causes a reduction in the level of glucose reaching the brain, but it can adapt to slight variations in available glucose. In the case of patients with repeated traumas, an increase in the intensity and frequency of symptoms is observed due to the cumulative effect of the traumas with the progressive decrease in the level of glucose available at the brain level.
It is essential to evaluate the symptoms that persist after the acute period, including
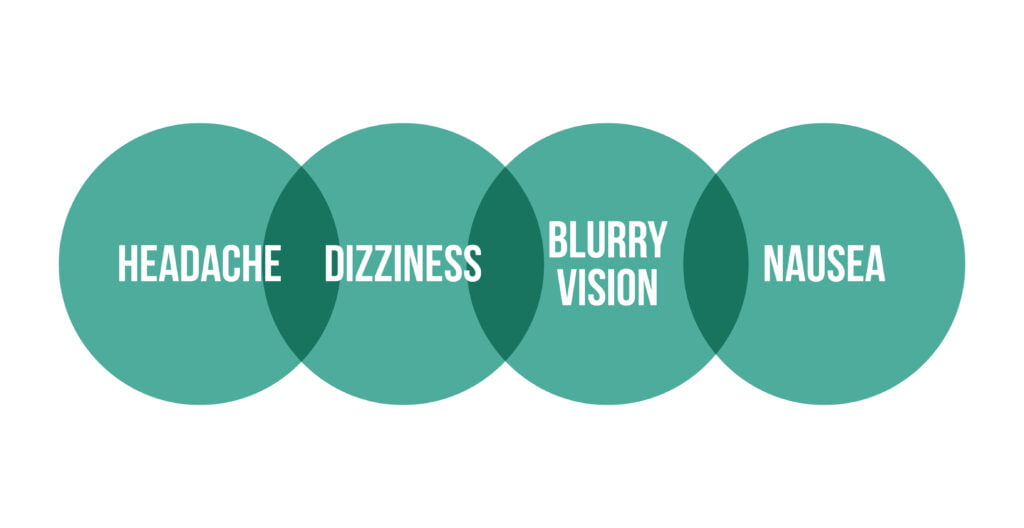
- Somatic symptoms: The most common symptoms in TBI patients are described in Figure 2. Usually, the symptoms disappear after a few hours in mild forms of TBI. Patients can also have seizures, balance, and mobilization disorders, and increased sensitivity to sounds and light. In the more severe forms of TBI, these symptoms usually disappear after 3-6 months [1, 3].
Symptoms post-TBI:
- Cognitive symptoms
- Memory problems (retrograde and anterograde amnesia)
- Word finding difficulty
- Attention and concentration troubles
- Psychological symptoms
- Anxiety
- Depression
- Poor self-esteem
- Feelings of worthlessness
- Behavioral symptoms
- Aggression
- Isolation.
How is CBIMI treated?
An over-the-counter way of treating brain fuel deficiency is the administration of glucose in the form of tablets, jellies, or a powder with dextrose added to a liquid. Glucose acts like this [1]:
- It bypasses the mechanism that limits glucose reaching the brain.
- Reaches the cerebral level and feeds the brain, responding quickly to the administered substances.
- 3-4 doses per day for 3-6 months may be required.
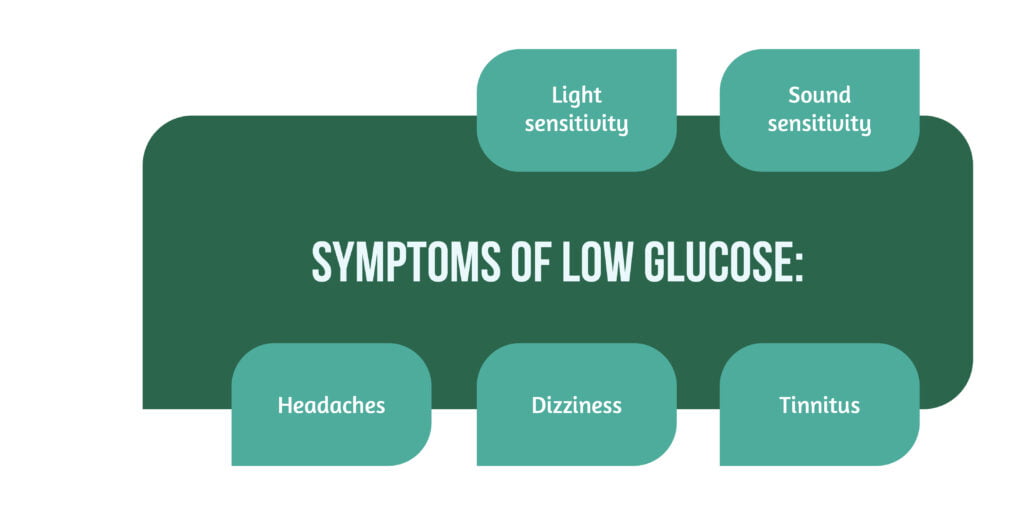
- When the glucose level drops below a certain level due to its use or stressful situations, certain symptoms may appear (Figure 3) [1].
- Gradually the factor that limits glucose from reaching the brain level decreases, and the amount of glucose produced by the body is higher, so the intake of exogenous glucose required decreases [1].
Cognitive-behavioral therapy (CBT) is essential in treating CBIMI to develop adequate mechanisms to overcome the traumatic event, helping the recovery process. Performing CBT without ensuring brain fuel in adequate quantities can give good results, but the process will be longer and with functional disorders in some brain areas [1].
Training of the peripheral physical systems should be started after a variable period of several weeks or months in which the cerebral glucose requirement has been ensured. Balance therapy helps reduce balance disorders and reduces the risk of falling. Vision training involves several sessions of performing exercises that should be continued at home to improve visual skills. However, starting this therapy too soon can worsen or exacerbate the headache [1].
Conclusion
Many studies aimed to understand the mechanism and consequences of concussions, brain trauma, and mental disorders without obtaining precise results. However, until now, no general rule of treatment or evolution of a TBI patient could be established. Therefore, TBI treatment must be individualized for each patient depending on the severity of symptoms, pre-existing pathologies, and complications.
Traumatic experiences activate the sympathetic nervous system, reducing the glucose that reaches the brain. The limitation of brain fuel is increased after each brain trauma, which is why the symptoms are more pronounced in patients with repeated TBI.
For more information about the impact of TBI visit:
- Immune response post-TBI
- How does TBI affect the functions of patients?
- Advances in TBI care and therapies
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
Bibliography
- Treatment of Brain Injuries and Mental Illness in Colorado Springs, CO | Peak Neuropsychology and Brain Rehabilitation. Available from: https://www.peakneuropsych.com/treatment-of-brain-injuries-and-mental-illness
- VanItallie TB. Traumatic brain injury (TBI) in collision sports: Possible mechanisms of transformation into chronic traumatic encephalopathy (CTE). Metabolism. 2019;100:153943. doi:10.1016/j.metabol.2019.07.007
- Katz DI, Cohen SI, Alexander MP. Mild traumatic brain injury. In: Handbook of Clinical Neurology. Vol 127. Elsevier; 2015:131-156. doi:10.1016/B978-0-444-52892-6.00009-X
- List J, Ott S, Bukowski M, Lindenberg R, Flöel A. Cognitive function and brain structure after recurrent mild traumatic brain injuries in young-to-middle-aged adults. Front Hum Neurosci. 2015;9. doi:10.3389/fnhum.2015.00228