Keywords: TBI, TBI and alcohol, alcohol use disorder, alcohol consumption, cognitive dysfunction in TBI, risk factors for TBI, alcohol consumption withdrawal
Focus keyword: alcohol consumption and TBI
What is the relationship between Alcohol Consumption and TBI?
Today when we speak about TBI, we have to also speak about alcohol misuse. The relationship between alcohol consumption and TBI has been established for a long time. Unfortunately, it continues to represent a significant problem, leading to substantial disability and death [1,2].
When referring to alcohol and TBI, we consider, on the one hand, the use of alcohol before TBI, leading to what is often called alcohol-related TBI, and on the other hand, alcohol consumption after TBI. The two situations have some essential differences [1]:
- Alcohol consumption represents a predictor for TBI since many cases of neurotrauma appear secondary to alcohol consumption
- TBI represents a risk factor and a modulating factor for alcohol use disorder.
What happens to the brain when using alcohol AFTER TBI?
Studies have shown that people who have suffered a TBI tend to have a higher sensitivity to alcohol, leading to a higher chance of suffering other TBIs when consuming alcohol. Furthermore, a significant aspect regarding alcohol consumption after TBI relies on the post-TBI cognitive dysfunction or emotional disability (e.g., depression), that leads to an increase in alcohol use. Additionally, consuming alcohol negatively affects rehabilitation after TBI. Therefore, for a person who has suffered a TBI, the rehabilitation and limitation of alcohol use are of utmost importance, for allowing the brain to heal [3].
Alcoholics have a higher risk of suffering a seizure, leading to falls and secondary TBI. Moreover, people who have suffered neurotrauma early in life tend to have a higher risk of developing substance misuse [3].
Learn more about Neurotrauma in the following articles:
- Prevention of Neurotrauma is the Best Treatment
- What is a Traumatic Brain Injury
- Can TBI affect emotions and behaviors?
What happens to the brain when using alcohol BEFORE TBI?
Alcohol consumption and TBI have been long correlated, with almost half of the patients being intoxicated at the time of injury. An even higher amount is revealed when considering TBI due to motor vehicle accidents and assault. Cyclists also have a higher rate of TBI when intoxicated.
It is estimated that the incidence of TBI can be up to 4x higher among individuals who drink and those who do not [1,3].
Given the incidence and correlation between alcohol consumption and TBI, several studies have been made, focusing on the blood level of alcohol at the time of TBI versus the survival and outcome of these patients. Unfortunately, the research presents inconclusive results [1,3].
Usually, in TBI patients, the period after the injury is characterized by a significant fall in alcohol consumption. The reasons vary greatly:
- Advice is given by physicians regarding alcohol abstinence in the early post-TBI phase to lessen as much as possible the onset of seizures
- Limitation of access to alcohol due to:
- Hospitalization
- Family
- Rehabilitation facility admission
- Cognitive impairments
- Physical impairments
- Own decision to stop drinking due to the occurrence of TBI in the context of alcohol consumption (e.g., suffering a TBI in a car crash in the context of alcohol consumption) [1,3].
Some patients manage to quit drinking permanently. Unfortunately, a significant number will resume misuse after some time, with part of them even increasing the amount of alcohol ingested in the years following TBI. For TBI patients with prior alcohol misuse, the risk for alcohol use disorder after TBI is higher. Nevertheless, what remains certain is that the use of alcohol increases the risk of suffering a TBI [3].
Why should the combination of alcohol and TBI be of concern?
The symptoms, cognitive dysfunction, and neuronal pathways that are lesioned during a TBI or alcohol misuse often overlap, making the diagnosis, differentiation of the cause, and clinical picture in patients with co-occurring TBI and alcohol use a complex and challenging matter [4] (Figure 1).
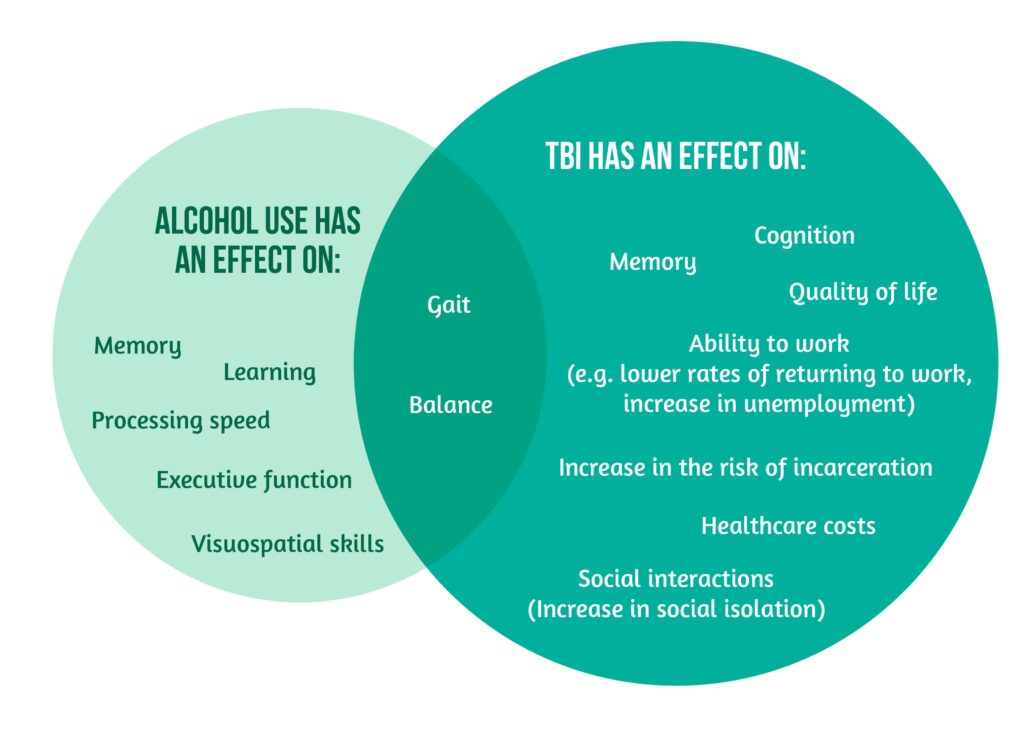
The correlation between TBI and alcohol use has several important implications for the patient concerning:
- Rehabilitation: the recovery after TBI is negatively affected by alcohol misuse; the effect ranges from extending the time needed for recovery to discontinuation. The brain needs time for healing, with the recovery happening even years after the TBI. Alcohol represents an obstacle in the path to recovery.
- Seizures: TBI patients have a higher risk of developing seizures. Alcohol not only elevates the risk of seizures, but can also trigger them.
- Subsequent TBIs: TBI patients have a higher risk of developing a new TBI. Patients with alcohol-related TBI have an even higher risk of experiencing a further TBI.
- Cognitive function: cognitive functions are affected by both TBI and alcohol. Unfortunately, TBI patients are more sensitive to alcohol compared to other people. Additionally, alcohol consumption can aggravate the post-TBI cognitive dysfunction, with its effect lasting up to weeks after cessation.
- Emotional state: depression is encountered more often in TBI patients than in the general population, while alcohol can lead to depression and aggravate it. Alcohol can suppress the effect of medications, which is why mixing alcohol with medication should be avoided.
- Sexual function: Sexual pleasure can be affected by alcohol consumption in men and women. The impact of alcohol use in men leads to erectile dysfunction, lower levels of testosterone, and reduced sex drive [1].
The prime actors in reducing harm and preventing future disability are the patients. They must understand that there is no safe use of alcohol after TBI. Therefore, it is essential to stop drinking for safety reasons and to ensure the recovery of the brain. If that is not possible, consuming alcohol in low doses remains the alternative. Furthermore, several suggestions can be used to reduce the harm of alcohol consumption:
- Drinking a maximum of two drinks per day, with a maximum of one drink per hour
- Eating and drinking before and after consuming alcohol
- Reducing vitamin deficiencies that appear secondary to alcohol use, like vitamin B1, B12, and folate, as they can have a negative impact on the brain
- Avoiding the consumption of beverages with high alcohol content
- Trying to have periods with absolutely no alcohol consumption [1, 5].
The second actors in reducing harm and preventing future disability are different institutions. These include organizations that create a safer environment and accessibility to quality healthcare without stigmatization.
TBI patients become more sensitive to alcohol, which is one reason why even a low amount of alcohol might harm [1].
Please contact your general physician or find local substance abuse or mental health facility for support!
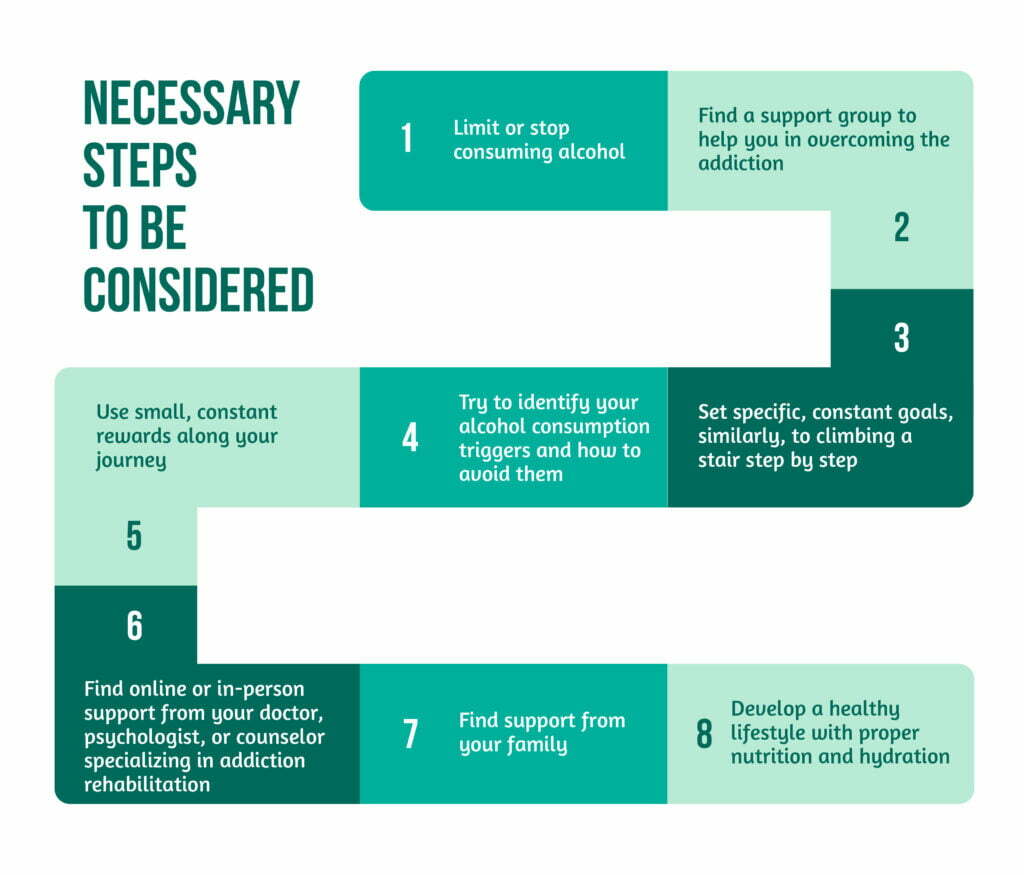
The steps that can be taken are showcased in Figure 2.
Alcohol consumption remains a taboo subject in today’s society, with increased stigma. However, it be surpassed. People can overcome alcohol misuse and have normal, limited alcohol consumption. Unfortunately, adding TBI to the context will further complicate the process.
The combination of TBI and alcohol makes people more sensitive to alcohol and hinders not only the recovery process of the brain, but also increases the disabilities mentioned above. For this, it is essential to understand the relationship of TBI with alcohol, access external resources, and help and set up a plan and commitment to overcoming this challenge.
People are different, so for some it might be a more challenging and lengthy process, but it is essential to start addressing problems on a personal level. Commitment combined with support from others, starting with family and friends is the key to success and a good quality of life.
Bibliography
- Bombardier CH, & Corrigan JD, in collaboration with the American Institutes for Research Model Systems Knowledge Translation Center. Alcohol use after traumatic brain injury, Model Systems Knowledge Translation Center, Jan 2021, available at: https://msktc.org/tbi/factsheets/Alcohol-Use-After-Traumatic-Brain-Injury#:~:text=Alcohol%20and%20traumatic%20brain%20injury,who%20did%20had%20worse%20outcomes.
- Weil ZM, Corrigan JD, Karelina K. Alcohol Use Disorder and Traumatic Brain Injury. Alcohol Res. 2018;39(2):171-180. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6561403/
- Weil ZM, Corrigan JD, Karelina K. Alcohol abuse after traumatic brain injury: Experimental and clinical evidence. Neurosci Biobehav Rev. 2016 Mar;62:89-99. DOI: 10.1016/j.neubiorev.2016.01.005.
- Herrold, AA, Sander, AM, Wilson, KV, et al. Dual Diagnosis of Traumatic Brain Injury and Alcohol Use Disorder: Characterizing Clinical and Neurobiological Underpinnings. Curr Addict Rep 2, 273–284 (2015). https://doi.org/10.1007/s40429-015-0078-3)
- Bartolomei-Hill L, Edmonston A, Maryland Traumatic Brain Injury Partner Grant, Uncovering the Connection The relationship between opioids and brain injury, harm reduction strategies through a Brain Injury Informed Lens, Maryland Department of Health, 2020, available at https://health.maryland.gov/bha/Documents/Brain%20Injury%20%20Harm%20Reduction%20Strategies.pdf