Keywords: TBI, brain, DAI, coma
Focus Keyword: TBI
What is a traumatic brain injury?
Traumatic brain injury (TBI) is defined by the Center for Disease Control and Prevention (CDC) as a lesion that disrupts the normal functioning of the brain. It can be caused by a blow, a bump, or a penetrating head injury. The injuries can be closed or open [1, 2]. External forces that might cause a TBI are gunshot wounds to the head, car accidents, or falls. However, losing consciousness is not something mandatory during a TBI [3].
TBI represents an important cause of disability, morbidity and mortality worldwide [4]. The CDC documented 2014 56.800 TBI-related deaths and 288.000 TBI-related hospitalizations in children and adults [1]. It is estimated that approximately 1.1 million patients are evaluated in the emergency department each year for acute TBI, mainly youth; the TBI incidence peak is at the ages of 15 to 24 years old [5].
For more information about brain injuries visit:
- Why is TBI a global burden?
- Prevention of Neurotrauma is the Best Treatment
- Concussions recovery after TBI – what is the process?
The following are the commonly accepted criteria established by the TBI Model Systems (TBIMS) to identify the presence and severity of a TBI:
Damage to brain tissue that is caused by an external force or at least one of the following:
- Amnesia – the person cannot recall the traumatic event
- A documented loss of consciousness
- Abnormal brain scan, skull fracture, or a post-traumatic seizure due to the trauma suffered
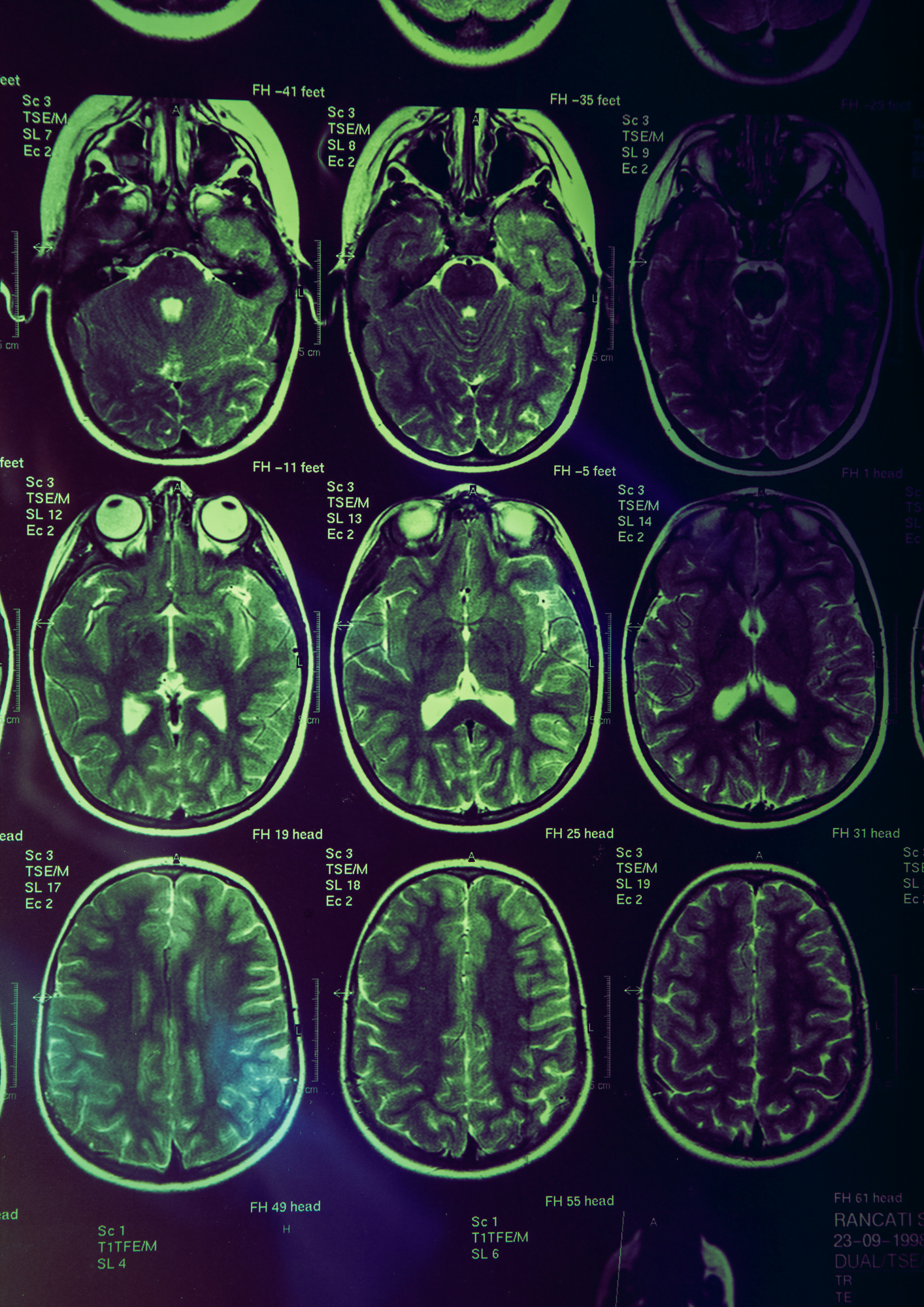
This model focuses especially on persons that suffered a moderate to severe TBI that require rehabilitation [Figure 1].

What types of injuries exist?
Because the brain is formed of soft and delicate tissue floating in the fluid within the skull, it can be very easily compressed, pulled, and stretched. In a car crash, the brain can move violently inside the skull, causing significant damage. Next, we will present the most representative types of injuries.
-
Closed versus open head injury
A closed injury means that the skull and brain contents have not been penetrated (primarily the result of a motor vehicle crash). In contrast, an opened injury means that the skull and other protective layers are penetrated and therefore exposed to air (for example, gunshot wounds). In a closed wound, the damage occurs because the person’s head stops abruptly. While moving, the brain collides with the skull. In a high-speed accident, the brain rotates inside the skull, thus damaging axons and blood vessels by stretching and tearing them. As a result, after a closed head injury, the damage can occur in a localized manner or spread throughout the brain (diffuse axonal injury).
After an opened head injury, the damage seems to be more localized. Depending on the destructive path of the bullet or other invasive object, damage can be similar to a closed injury.
-
Primary versus secondary injury
The injuries that occur at the time of injury are primary injuries and cannot be reversed. The main goal of hospitalization and acute management is to prevent any further secondary injury to the brain. The types of primary injuries are showcased in Figure 2.

Secondary injuries usually appear a few days after the initial injury. They can be due to a lack of oxygen to the brain, which can result from low blood pressure or increased intracranial pressure from brain tissue swelling.
How to grade the severity of a TBI?
The extent of brain tissue damage is characterized by the severity of the injury. This is estimated by measuring different parameters such as:
- duration of consciousness loss
- the depth of coma
- level of amnesia
- brain scans
The depth of the coma is measured using the Glasgow Coma Scale (GCS), which appreciates three functions (eye opening, verbal response and movement). Using the GCS coma, patients are ranked as:
- a score of 3 (lowest possible score) indicates a profound coma
- a score of 9 signifies that the person is no longer in a coma
- a score of 15 (highest possible score) means that the person is fully conscious.
The need for intubation is decided by calculating the GCS. The score is recalculated during recovery. The post-traumatic amnesia duration is another good estimate of the brain injury severity, the longer the duration, the more severe the damage to the brain. Post-traumatic amnesia is characterized by intellectual and behavioral disturbances, presented in Figure 3 below [6].

CT or MRI scan?
CT scans are often used for moderate to severe TBI patients to evaluate the evolution of lesions. Depending on the patient’s lesions, magnetic resonance imaging (MRI) can also be done. One must keep in mind that not all lesions can be detected by imagery.
Recent studies showed that the MRI has proven superior for every pathology besides subarachnoid haemorrhage and skull fracture. However, CT scans remain the most commonly used imaging option after a TBI due to their rapidity and the ability to easily scan the abdomen, chest and spine for traumatic injuries [7].
How does the brain tissue respond to injury?
Common problems that might appear in a TBI patient:
- increased intracranial pressure – due to the swelling of the brain due to the injury. It can also amplify brain damage.
- function of neurochemical problems that disrupt functioning – neurotransmitter imbalance might appear after a TBI. If treated promptly, the patient improves significantly.
- neural plasticity of the brain – represents the ability of the brain to adapt and change with time. This process starts immediately after an acute injury and lasts afterwards. It implies neuronal proliferation and synaptogenesis. Furthermore, all the new markers favor the remodelling and cortical changes that would subsequently favor recovery [8]. However, all these mechanism changes take time, and are directly correlated with clinical recovery pace.
Bibliography
- Capizzi A, Woo J, & Verduzco-Gutierrez M. ‘Traumatic Brain Injury’, Med. Clin. North Am. 2020, doi: 10.1016/j.mcna.2019.11.001.
- ‘Get the Facts About TBI | Concussion | Traumatic Brain Injury | CDC Injury Center’, Mar. 21, 2022. https://www.cdc.gov/traumaticbraininjury/get_the_facts.html
- ‘Understanding TBI: Part 1 – What happens to the brain during injury and the early stages of recovery from TBI? | Model Systems Knowledge Translation Center (MSKTC)’. https://msktc.org/tbi/factsheets/Understanding-TBI/What-Happens-During-Injury-And-In-Early-Stages-Of-Recovery
- Ng SY & Lee AYW. Traumatic Brain Injuries: Pathophysiology and Potential Therapeutic Targets, Front. Cell. Neurosci. 2019, doi: 10.3389/fncel.2019.00528.
- Heegaard W & Biros M. Traumatic brain injury, Emerg. Med. Clin. North Am.2007, doi: 10.1016/j.emc.2007.07.001.
- Ahmed S, Bierley R, Sheikh JI, Date ES. Post-traumatic amnesia after closed head injury: a review of the literature and some suggestions for further research, Brain Inj. 2000, doi: 10.1080/026990500421886.
- Bruce DA, ‘Imaging after head trauma: why, when and which’:, Childs Nerv. Syst. 2000, doi: 10.1007/PL00013720.
- YR SS, Veeravagu A, & Grant G. (2015). Neuroplasticity after traumatic brain injury. Available at: https://www.ncbi.nlm.nih.gov/books/NBK326735/