Authors: Iulia Vadan, Silvina Ilut
Keywords: TBI, headaches
Focus Keyword: Headaches
Over a third of patients who suffered a moderate or severe traumatic brain injury (TBI) and complain of headaches associated with TBI lasting for an extended period after the traumatic event. This makes it hard for them to concentrate on their daily activities and may cause difficulty in thinking and remembering things [1].
It is one of the most commonly reported symptoms and often one of the most persistent [2]. Its prevalence is usually varying between 30% and 90%. Of these patients, 18% to 22% of patients reported post-traumatic headache after one year [3].
What are the causes and most frequent types of headaches associated with TBI?
It is considered that headaches might appear due to various causes, as highlighted in Figure 1.:
- surgery
- skull fractures
- intracerebral hemorrhage
- medication side effects
- incomplete healing of the brain
- neck or skull injuries
- tension or stress

What are migraine headaches?
After a TBI, the patient may have migraine headaches because areas of the brain become hypersensitive, and as a result, they can trigger a pain signal that spreads out to other parts of the brain. The characteristics of migraine headaches are highlighted in Figure 2 below.

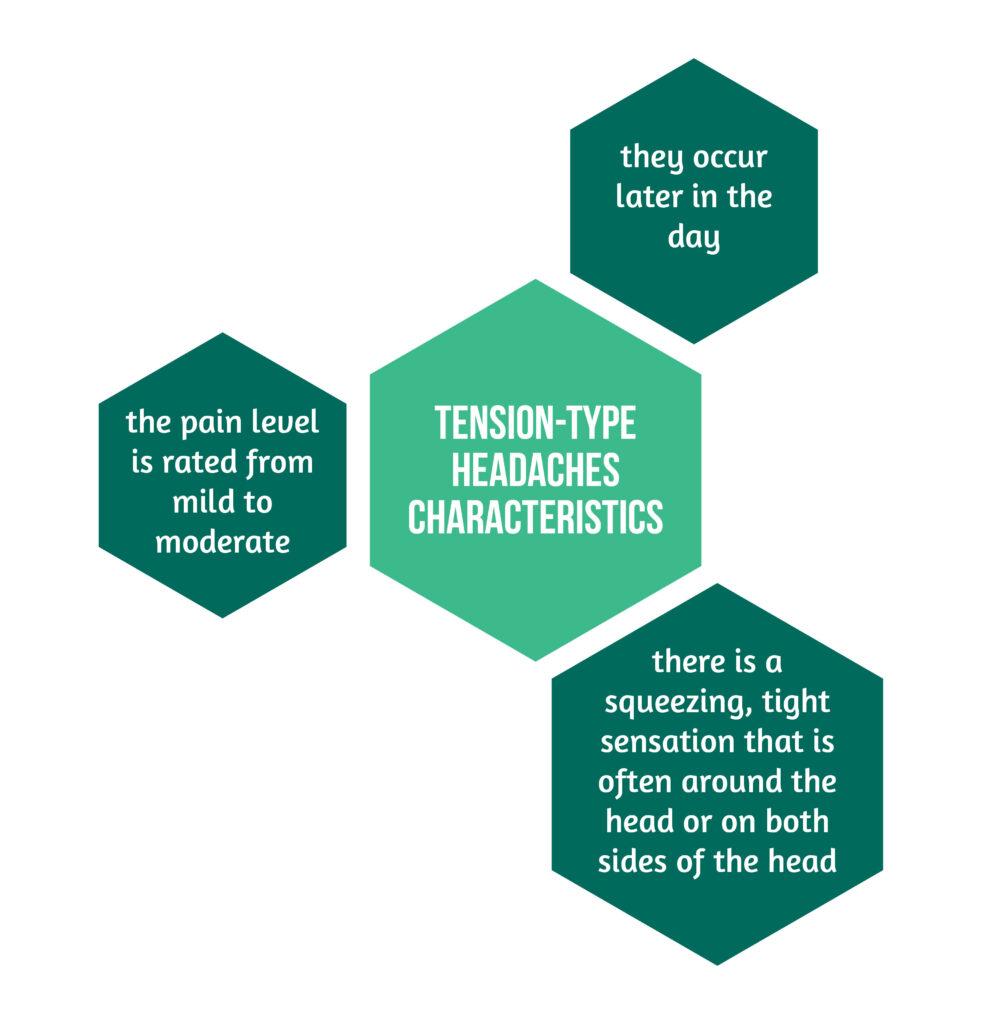
Tension-type headaches
These headaches are associated with stress or muscle tension and hold several characteristics, as showcased in Figure 3 below.
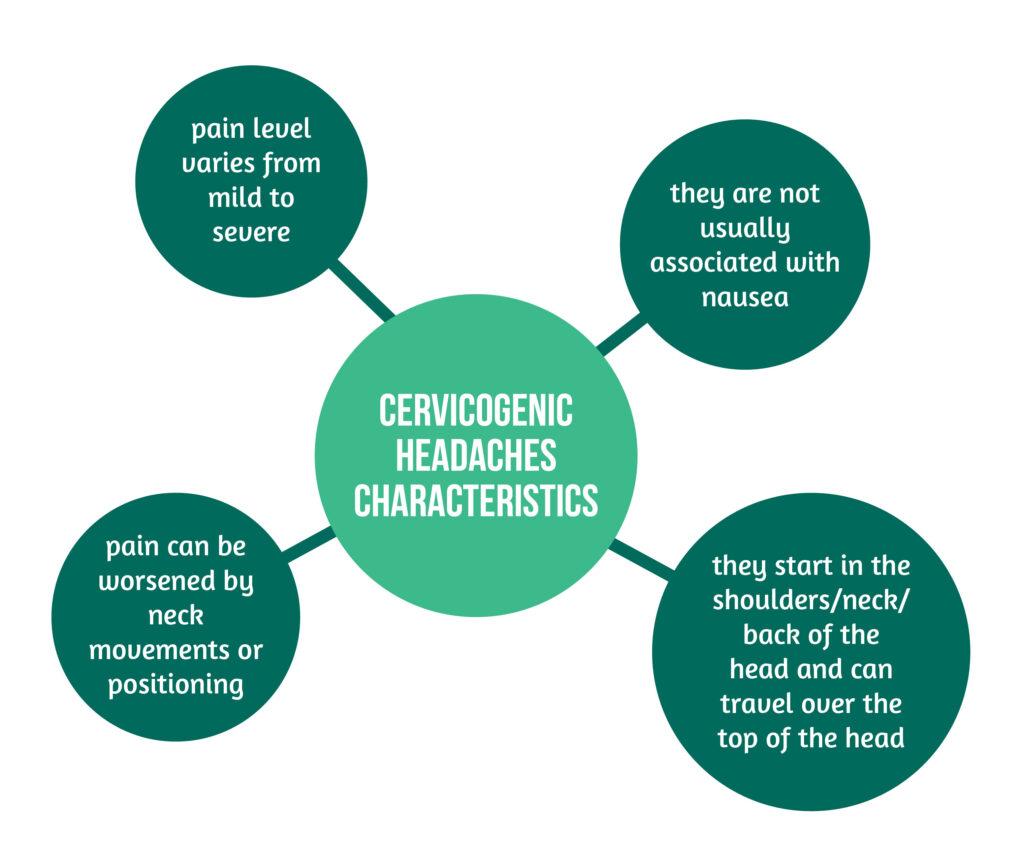
Cervicogenic headaches
Injury to the soft tissues and muscles in the neck and the back may cause cervicogenic headaches. This is because there are many nerves located there. The pain could be caused by their branches that are traveling through the skull and scalp. Cervicogenic headaches are characterised by several variables, underlined in Figure 4 below.
Rebound or medication overuse headaches
Rebound or medication overuse headaches are important to be recognized because many medicines used for treating brain injury can cause headaches. For example, a sudden decrease in caffeine/energy drinks/tea intake may cause rebound headaches. Medication overuse headaches might appear as a side effect of patients’ medicine. On the other hand, missing doses of certain medications can cause headaches.
Although these are the most common types of headaches, patients may complain of more than one type of headache after a TBI. Also, a pre-existing headache may worsen after a brain injury. This supports the theory that states that some factors associated with TBI might worsen or trigger headaches (for example, sleep apnea or vision problems).
More information on headaches after TBI will be available in a future blog post!
Headaches are not the only consequences of a TBI! Find out more on: “What happens after a TBI?”
If you wish to get different perspectives on the effects of neurotrauma from world-class specialists, visit the interviews from the Neurotrauma Treatment Simulation Center (NTSC) Vienna 2022:
Prof. Johannes Vester (AMN President): https://brain-amn.org/ntsc-interviews-series-johannes-vester-amn-president/
Prof. Christian Matula (Vienna General Hospital) : https://brain-amn.org/ntsc-interviews-series-christian-matula-meduni-wien-austria/
Prof. Peter Lackner (Klinik Floridsdorf): https://brain-amn.org/ntsc-interviews-series-peter-lackner/
Prof. Andreas Winkler (Klinik Pirawarth): https://brain-amn.org/ntsc-interviews-andreas-winkler/
Dr. Daniel Csomor (Landeskrankenhaus Wiener Neustadt): https://brain-amn.org/ntsc-interviews-daniel-csomor/
References
1. Howard L & Schwedt TJ. Posttraumatic headache: recent progress. Curr. Opin. Neurol.2020; 33, 316–322. https://pubmed.ncbi.nlm.nih.gov/32304441/
2. Lucas S, Hoffman JM, Bell KR, Walker W & Dikmen S. Characterization of headache after traumatic brain injury. Cephalalgia Int. J. Headache 2012; 32, 600–606. https://pubmed.ncbi.nlm.nih.gov/22623761/
3. Tessler J & Horn L. J. Post-Traumatic Headache. in StatPearls (StatPearls Publishing, 2022) https://www.ncbi.nlm.nih.gov/books/NBK556134/




