Keywords: TBI, sports, concussion, CTE, chronic traumatic encephalopathy
What is Chronic Traumatic Encephalopathy?
Traumatic brain injury (TBI) represents one of the most important pathologies worldwide. Studies show that the incidence rate of TBI in the US is 579 per 100,000 persons, with approximately 1,7 million cases each year on all levels of the TBI severity [1]. It is considered that mild TBIs represent 80% of the total of these injuries [2]. TBI interferes with the usual way the brain works, causing different problems depending on which parts of the brain are most damaged [3].
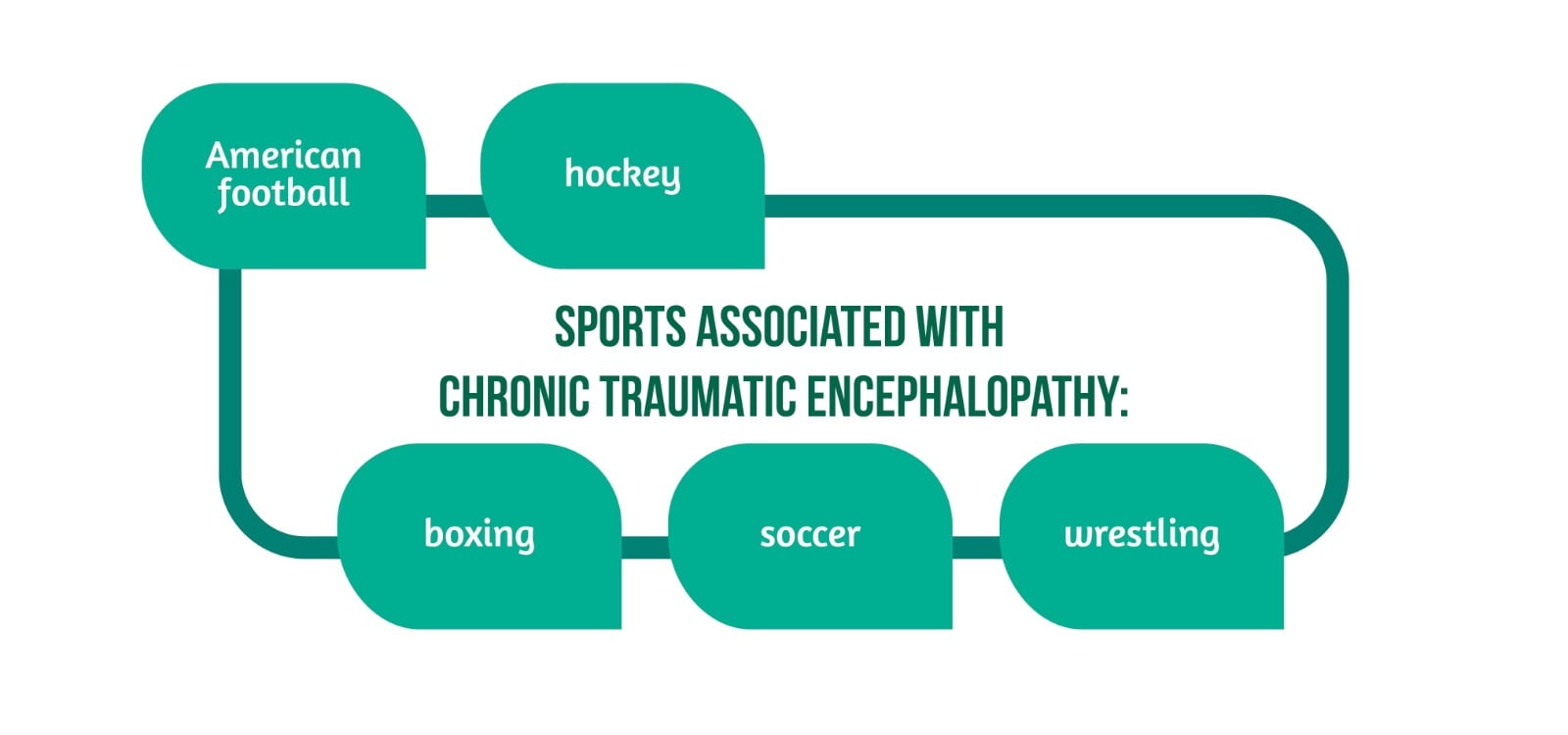
One of the critical post-traumatic pathologies is represented by chronic traumatic encephalopathy (CTE), a progressive brain condition that is a result of repeated episodes of concussion as a consequence of repeated blows to the head. Previously known as “dementia pugilistica” or “punch drunk” syndrome, today, these terms are no longer used because it is proven that this pathology is not linked only to ex-boxers [4]. However, it has become a popular topic due to its association with several sports (Figure 1).
Many retired athletes show problems with anger, memory, substance abuse, or depression. Scientists consider that there is a link between these cognitive, emotional, and physical manifestations and CTE [5]. However, debate still exists on how diagnostic criteria should be used for CTE, and current treatment is only supportive. The current literature mainly focuses on finding the best way to diagnose and treat CTE.
What are the symptoms of CTE?
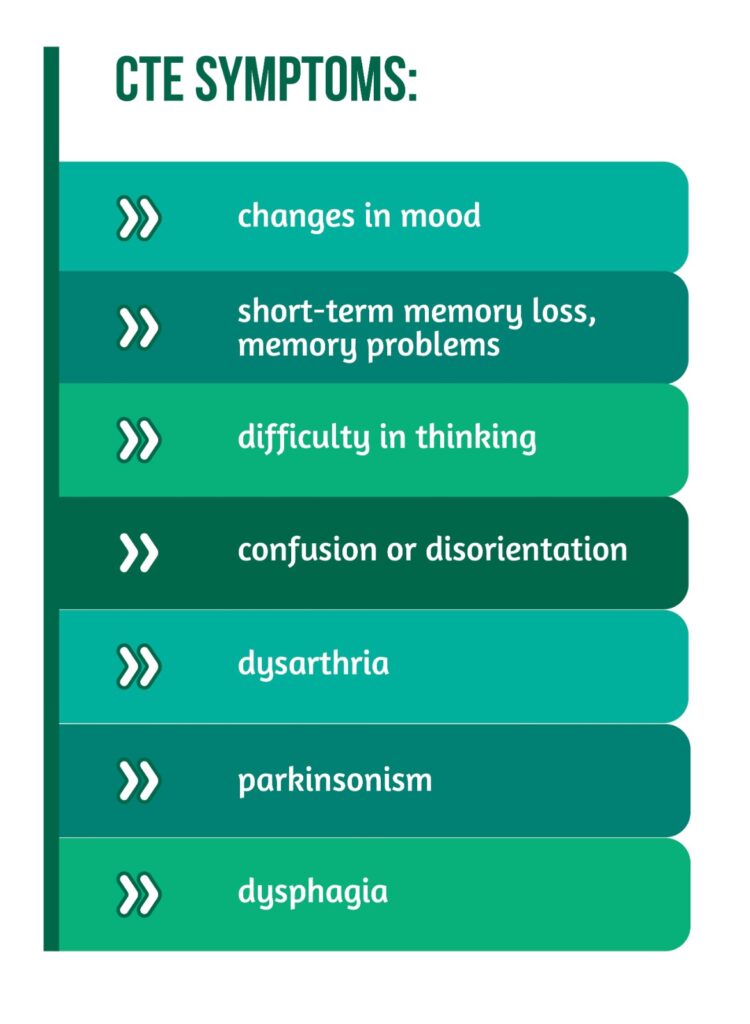
The symptoms of CTE vary but tend to be similar to those of other neurodegenerative conditions such as Alzheimer’s disease. They usually start several years after receiving repeated blows to the head or suffering from repeated concussions and can ultimately lead to dementia due to their repercussions on brain functioning. Some of the symptoms are presented in Figure 2.
The mood changes are marked by depression, frequent mood swings, and feelings of anxiety or agitation. The short-term memory loss is revealed by patients asking the same question repeatedly or having difficulty remembering people or phone numbers. Confusion or disorientation is showcased by getting lost frequently and not knowing the day of the week, while parkinsonism by tremors, muscle stiffness, and slow movement.
What are the causes of CTE?
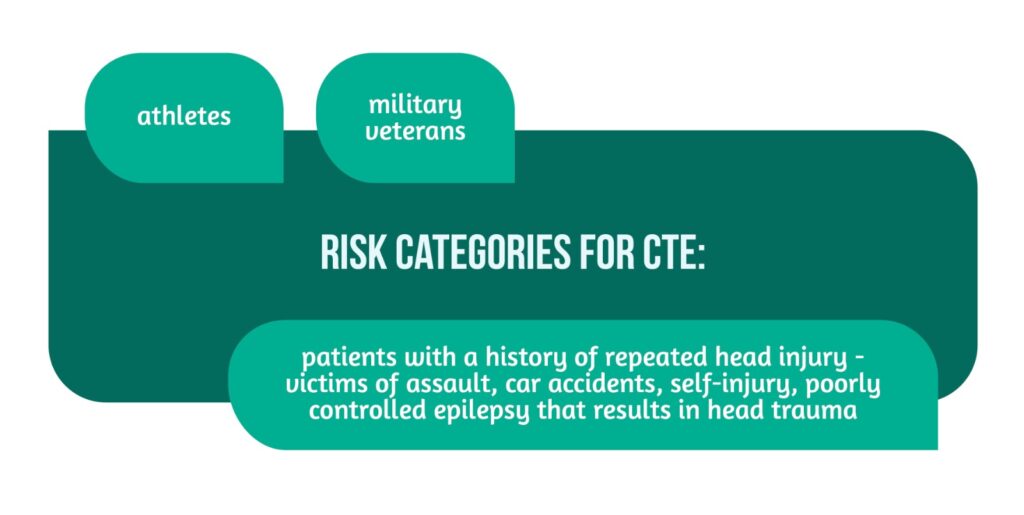
Any activity that implies recurrent episodes of concussion or repeated blows to the head is thought to increase the risk of CTE development in the future. The most at-risk categories are presented in Figure 3 [4].
When should someone get medical advice?
Any patient who is worried about memory can address their concerns by seeing their general practitioner (GP). If the person is worried about someone else, they should encourage them to make an appointment and offer to accompany them to the consult.
It is essential to keep in mind that there can be other causes for memory problems [4]:
- stress
- depression
- medication
- other health problems.
The GP is the first medical professional that carries out a check-up of the patient tries to find out what the cause can be, and refers them, if needed, to a specialist that can apply more tests.
How is CTE diagnosed?
Currently, there is no available test to diagnose Chronic Traumatic Encephalopathy. Therefore, the patient’s history remains the most crucial helper for the specialist. The patients who practiced contact sports remain the most at-risk group for this pathology and should be thoroughly examined.
The GP might start the consult by giving the patient simple mental tasks such as walking around. They can refer the patient to a specialist for a detailed memory assessment if needed. Routine brain scans might not help diagnose CTE as the results can be similar to those in similar conditions. The only certain way to diagnose CTE is a post-mortem examination. Studies suggest that the changes in the brain of CTE patients are different from those of patients who suffer from Alzheimer’s disease. Even so, there are some similarities between them, such as the presence of:
- tau protein
- brain atrophy (shrinking of the brain)
- neurofibrillary tangles.
Magnetic resonance imaging and Computed tomography scans are the most used tests for investigating and diagnosing neurodegenerative pathologies [4]. The damage suffered by the axons due to repetitive TBIs can cause changes in the membrane permeability and alter ionic shifts causing a large influx of calcium. As a result, there is a release of calpains and caspases that trigger the phosphorylation of the tau protein, its shortening, misfolding, and aggregation, and the failure of the cytoskeleton with the dissolution of the microtubules and neurofilaments [5, 6].
What is the conclusion?
CTE represents a complex neurodegenerative disease that is a consequence of repetitive closed-head injuries for which there is no current specific diagnostic test or specific treatment. The exact mechanism of onset is not fully understood, but there are some categories of patients that are predisposed to developing this pathology (athletes, military veterans, etc.).
More and more research is focusing on answering all of the questions as clearly and concisely as possible to obtain an easier and more concrete diagnostic test and treatment in the future. What remains clear is that any persons suffering from memory problems or friends and family who know someone having these symptoms should discuss with a medical specialist to obtain a proper examination and exclude other possible causes or health problems that might cause these issues.
For more information about the impact of TBI visit:
- Boston University Center for the Study of Traumatic Encephalopathy contribution to understanding this disease
- How does TBI affect the functions of patients?
- Advances in TBI care and therapies
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
Bibliography
- Faul M and Coronado V. ‘Epidemiology of traumatic brain injury’, Handb. Clin. Neurol. 2015, vol. 127, pp. 3–13, doi: 10.1016/B978-0-444-52892-6.00001-5.
- Ponsford J, Cameron P, Fitzgerald M, Grant M, and Mikocka-Walus A. ‘Long-term outcomes after uncomplicated mild traumatic brain injury: a comparison with trauma controls’, J. Neurotrauma 2011, doi: 10.1089/neu.2010.1516.
- ‘Understanding Traumatic Brain Injury Part 2: Brain injury impact on individuals’ functioning’, p. 4. Available from: https://msktc.org/tbi/factsheets/understanding-tbi-part-2-brain-injury-impact-individuals-functioning
- ‘Chronic traumatic encephalopathy’, nhs.uk, 2017. https://www.nhs.uk/conditions/chronic-traumatic-encephalopathy/ (accessed Nov. 16, 2022).
- Saulle M and Greenwald BD. ‘Chronic Traumatic Encephalopathy: A Review’, Rehabil. Res. Pract. 2012, doi: 10.1155/2012/816069.
- Gavett BE, Stern RA, and McKee AC. ‘Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma’, Clin. Sports Med. 2011. doi: 10.1016/j.csm.2010.09.007