Keywords: traumatic brain injury, children, pediatric TBI, pediatric mild TBI, school, treatment, neuropsychological assessment, disability
How does traumatic brain injury impact children?
Traumatic brain injury (TBI) leads to lesions that can be diffuse, focal, or both. The signs and symptoms following the trauma are diverse following the extent of the lesions, localization, and age of the child. Furthermore, considering the continuous development of the brain during childhood, the functional consequences of TBI are different compared to adults. Similar to TBIs in adults, the severity of TBI (mild, moderate, severe) is determined by the extension and type of injury, posttraumatic amnesia, and length of the loss of consciousness [1–3].
Signs and symptoms might change and become apparent in time, especially when the child is stimulated during different activities and cognitive processes. The impairments might become evident, especially during the school [1–3].
Pediatric TBI is a significant cause of mortality and disability. Although the lesions post-TBI might be comparable to those in adults, several aspects are different, mainly due to differences related to age (e.g., anatomy, physiology, physio-pathological responses, pattern of lesions, neurological signs, and symptoms). For example:
- a small quantity of blood might lead to hemorrhagic shock in a small child
- the child’s capabilities highly influence the neurological evaluation
- long-term evaluation of the child might be needed to assess the outcomes (physical and mental) [2].
Post-moderate and severe TBI children have an increased risk of developing adaptive-functioning difficulties, reduced performance in educational activities, and behavioral and emotional disabilities [3].
Most TBIs in children are mild. They frequently do not require hospital admission and the presentation to medical specialists is variable, thus making an accurate evaluation of outcomes and level of disabilities post mild TBI difficult. Nevertheless, the overall outcome is primarily good, despite headaches, cognitive and behavioral signs, and symptoms during the early post-TBI stage. Unfortunately, some patients might present these disabilities long-term [4].
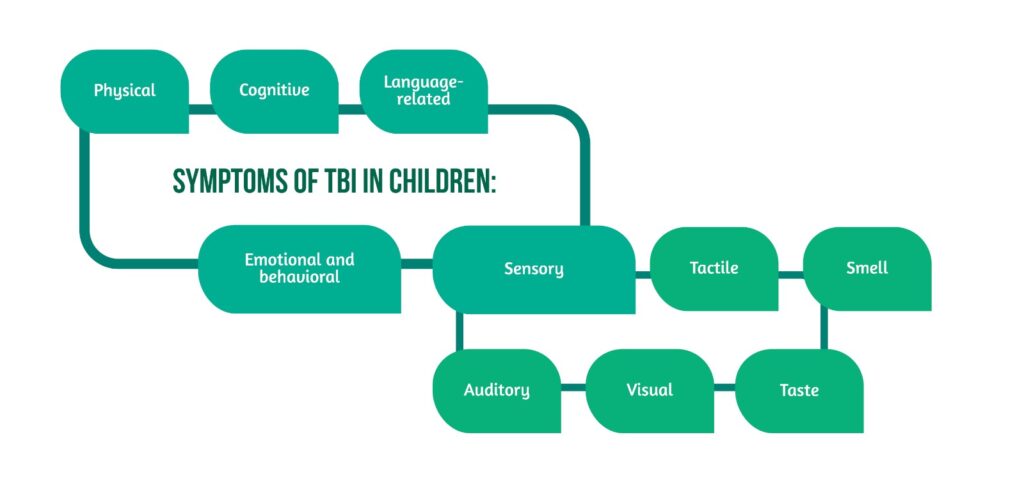
What are the signs and symptoms of TBI in children?
Depending on the type of TBI, a large variety of signs and symptoms might be encountered post-injury:
Physical
- motor deficits
- disorders of consciousness
- disorder with balance and coordination
- headache
- pain
- seizures
- nausea and vomiting
- swallowing difficulty
- slowed reaction time.
Sensory
- Auditory: hearing loss, hyperacusis, tinnitus
- Visual: loss/reduced visual acuity, photophobia, visual field defects
- Taste: loss of taste
- Smell: loss of smell
- Tactile: increased sensitivity to touch, pain, or/and temperature.
Cognitive
- Attention deficit
- Memory deficits
- Disorientation
- Difficulty in judgment, planning and organizing activities, making decisions, solving problems, learning.
Language and vocal
- Impaired fluent speech
- Dysprosody
- Dysarthria
- Difficulties in using some words
- Difficulty understanding abstract elements of language
- Difficulty understanding written text, especially complex texts
- Trouble holding a conversation
- Difficulties using and understanding non-verbal communication (body language, voice tonality, facial mimic)
- Inability or impaired ability to speak
- Qualitative modifications of the voice (hoarseness, nasal or high-pitched voice).
Emotional and behavior
- Anxiety
- Depression
- Agitation
- Aggression
- Lack of motivation
- Emotional instability
- Increased frustration
- Impulsivity
- Irritability
- Brain “fog” [3, 5] (Figure 1).
How do the consequences of TBI impact their daily activities, including in school?
The effects of TBI impair their daily activities and can be highlighted during school activities (Figure 2).
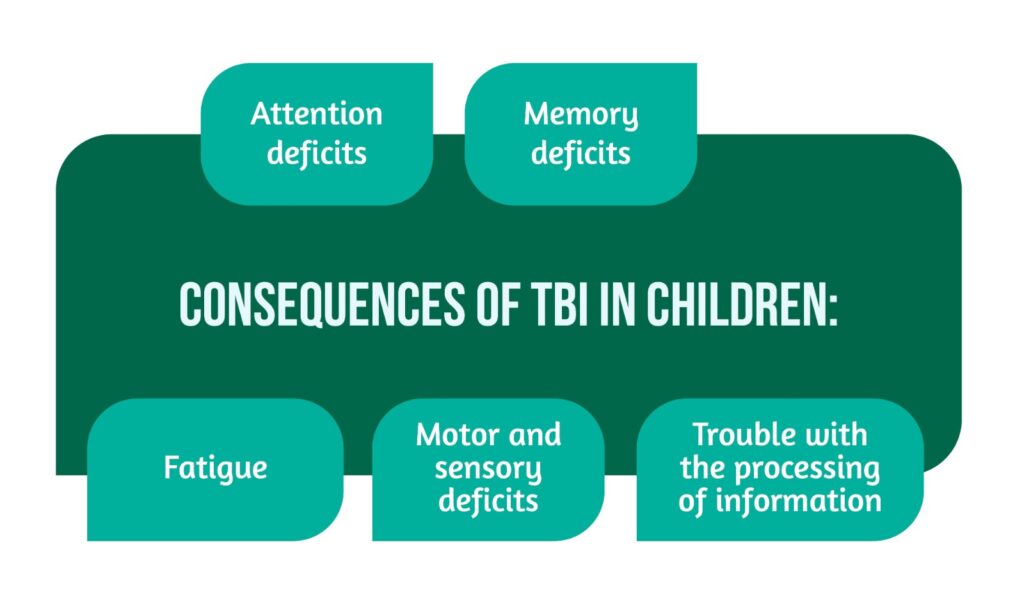
Furthermore, children with impulsive behavior and difficulties with concentration are considered to be at a higher risk of developing TBI.
Considering the increasing demands from children, especially regarding their performance in school, optimal management of the consequences of TBI is essential. Moreover, special attention should be given to children who have experienced a mild TBI. These might lack obvious signs of disability, leading parents to demand the same performance in school as before the TBI. However, it is essential to know that some signs might be subtle and, thus, interpreted as misbehavior or lack of motivation (for example, distractibility, restlessness, irritability) [2, 5].
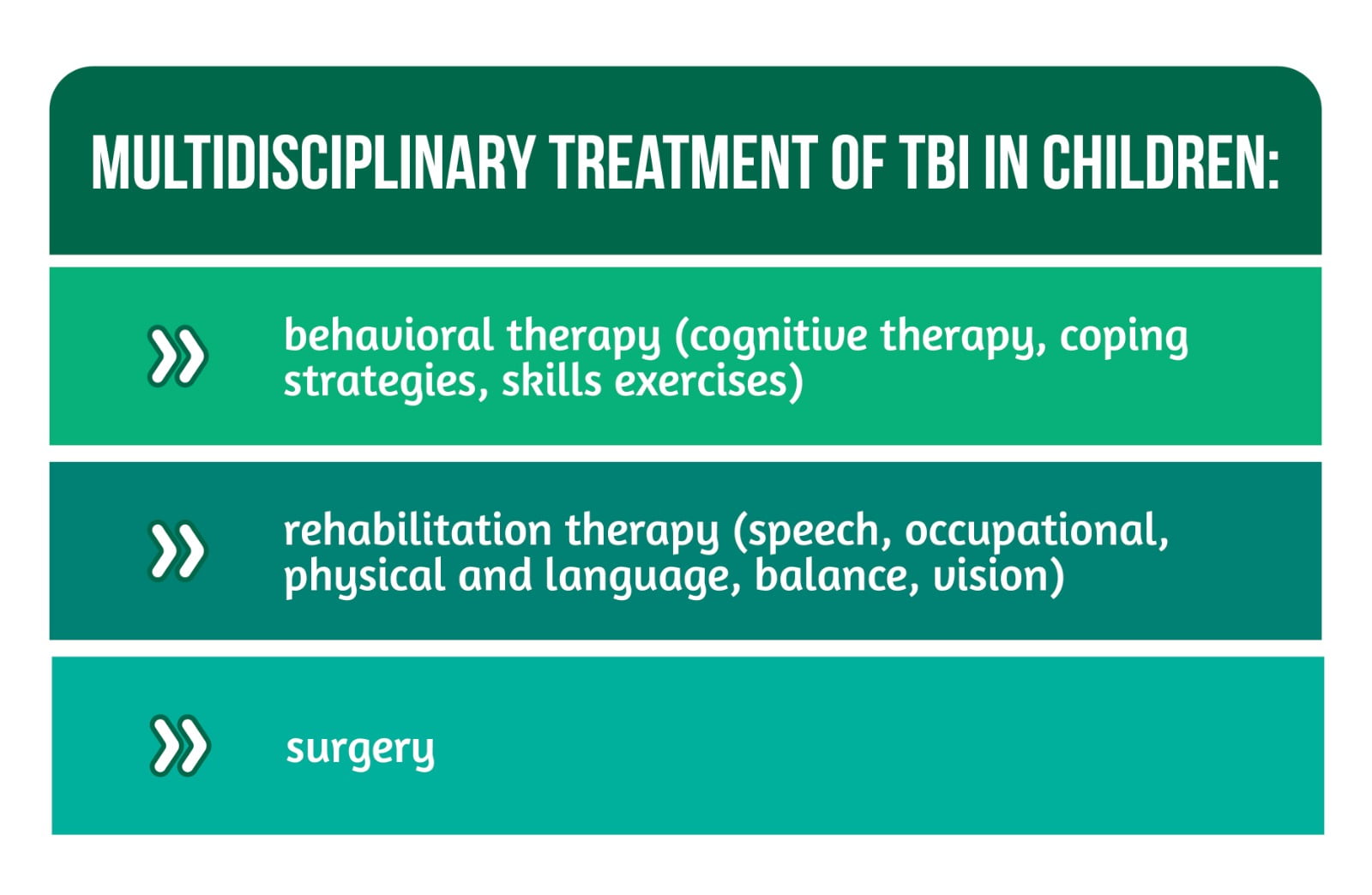
How can children be supported?
It is essential for children who have suffered a TBI to receive support from their families, rehabilitation professionals, as well as school personnel. Treatment of TBI in children should be multidisciplinary [5] (Figure 3).
How to prepare for the return to school?
Depending on the severity of TBI and disabilities, the time between the TBI and return to school varies. Following a collaboration between rehabilitation professionals, families, and school representatives, several aspects are analyzed, and the most suitable ways to ensure an easy accommodation for the child are determined (including current strengths, abilities inabilities, and difficulties). Several aspects should be considered before returning to school:
- Starting with partial time spent at school (not a complete day)
- Constant breaks for resting
- More time for homework or assignment completion
- Following the child’s behavior and emotions (identifying stress and mood changes)
- Paying attention to the possibility of the development of posttraumatic stress disorder [6].
The school personnel should be involved in rehabilitating and accommodating the student and several elements should be considered regarding the schools:
- Specially trained teachers can be used if needed
- Specific laws are in place to ensure that schools provide appropriate services for children with disabilities
- Teachers should be informed about the state of the child regarding the existing disabilities and adapt, offer additional help in and out of the day-to-day classes
- Teachers should determine together with neuropsychologists if the child can take part in all types of activities and if the grade is adequate considering the state of cognition; compare the child’s status before and after TBI
Evaluation of the following should be assessed while at school:
- Cognitive status: memory, learning, planning, self-evaluation, speed of thinking
- Social skills: emotional state, communication, behavior
- Physical abilities: power, coordination, balance, stamina
- Negative behaviors secondary to different triggers should be expected, and teachers should try to talk and understand their cause. For example, these might appear due to over-stimulation, unexpected events, or negative feedback.
What are the takeaways regarding TBI in children?
Functional consequences of TBI are different compared to adults. Signs and symptoms might change and become apparent in time, highlighting the need for optimal multidisciplinary management for children who suffer a TBI. Support from the family, rehabilitation professionals, as well as school personnel, is a vital need to ensure proper rehabilitation. Moreover, the involvement of informed school personnel is essential for rehabilitation and accommodation. Finally, continuous evaluation in school is vital to identify needs and adapt activities and demands accordingly [1–3, 4–6].
For more information about the impact of TBI visit:
- Boston University Center for the Study of Traumatic Encephalopathy contribution to understanding this disease
- How does TBI affect the functions of patients?
- Advances in TBI care and therapies
We kindly invite you to browse our Interview category https://brain-amn.org/category/interviews/. You will surely find a cluster of informative discussions with different specialists in the field of neurotrauma.
Bibliography
- Araki T, Yokota H, Morita A. Pediatric Traumatic Brain Injury: Characteristic Features, Diagnosis, and Management. Neurol Med Chir (Tokyo). 2017;57(2):82-93. doi:10.2176/nmc.ra.2016-0191
- Wehman P, Targett P, Ed M. Model Systems Knowledge Translation Center, Baylor Institute for Rehabilitation et al. Model Systems Knowledge Translation Center. Returning to school after Traumatic Brain Injury; c:2010; Available from: https://msktc.org/tbi/factsheets/returning-school-after-traumatic-brain-injury
- Taylor HG, Yeates KO, Wade SL, Drotar D, et al. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. 2002;16(1):15-27. doi:10.1037//0894-4105.16.1.15
- Ponsford J, Willmott C, Rothwell A, et al. Impact of early intervention on outcome after mild traumatic brain injury in children. Pediatrics. 2001;108(6):1297-1303. doi:10.1542/peds.108.6.1297
- American Speech-Language-Hearing Association. c2022. Pediatric Traumatic Brain Injury. Available from: https://www.asha.org/practice-portal/clinical-topics/pediatric-traumatic-brain-injury/#collapse_4
- Cincinnati Children’s. c2022. Traumatic Brain Injury in Children; 2021. Available from: https://www.cincinnatichildrens.org/health/t/traumatic-brain-injury




