Keywords: TBI rehabilitation, CENTER-TBI, access to TBI rehabilitation, TBI disability, TBI outcome, rehabilitation need for TBI
Introduction – TBI and TBI rehabilitation
The severity and disability after traumatic brain injury (TBI) are varied and frequently understated. The array of disabilities can be temporary or permanent, ranging from:
- physical symptoms and signs (motor deficit, dizziness, nausea, problems with sleep, headache)
- cognitive dysfunction (attention, memory, learning, or language disorders)
- emotional dysfunction (aggression, anger, irritability)
- mood dysfunction (anxiety, depression)
- behavioral and personality changes.
Overall, TBI leads to a decrease in the quality of life, affecting not only the individual, but also the family and close environment. Considering the web of symptoms and signs of TBI and the long-term impact of the secondary disability, a detailed assessment of TBI patients is essential to tailor the management, treatment, and rehabilitation according to the severity of the TBI and individual characteristics of the patient. The rehabilitation process is critical for improving patient outcomes. Given the complexity of TBI, there is an essential necessity for multidisciplinary rehabilitation teams to address the complex needs and disabilities of TBI patients in an individualized manner according to their needs [1-3].
Unfortunately, in clinical practice, during the acute phase of TBI, the multidisciplinary teams are lacking, with the types of rehabilitation more frequently covered being the physical, occupational, language, and speech therapies – and these, for a limited period, without addressing the patients need on an individual level. This is why for several TBI patients the rehabilitation needs are not covered.
Research on the matter led to divergent and inconclusive results. The needs vary according to the demographics and severity of the TBI. The sociodemographic factors predicting the need and level of use of rehabilitation could not have been established, with contrasting results regarding the sex and age of the patients receiving more rehabilitation. The severity of TBI and disability of patients is correlated with the use of rehabilitation. However, for TBI patients with less significant disabilities, the rehabilitation was insufficient [1,2,4].
The results of several studies suggest that access to rehabilitation after TBI is influenced by geographical factors mirrored in differences on healthcare policies establishing acute and referral to rehabilitation, as well as culture. Still, considering that most of the research is done in the US, further studies should be conducted internationally to overcome these limitations [1–5].
For more information on TBI rehabilitation, visit:
Moreover, check out the NTSC Interview with the rehabilitation specialist Professor Andreas Winkler from Klinik Pirawarth, Austria.
The CENTER-TBI Project
The Collaborative European NeuroTrauma Effectiveness Research focusing on TBI (CENTER-TBI) has enriched the European research regarding this pathology bringing it to an international level. An example of geographical and knowledgeable collaboration, methodology, and dedication, CENTER-TBI brought new insights about TBI at European level (also including Israel). The observational study ran for 3 years in multiple centers from 17 European countries and Israel, leading to the publication of several results, including a prevalence of rehabilitation during the first-year post-TBI of about one-third across the studied TBI population covering all levels of TBI severity and identification of predicting factors for access to TBI rehabilitation [1].
CENTER-TBI: Focus on Rehabilitation
The need for rehabilitation and allocation of rehabilitation is done for patients with functional limitations and moderate to severe disabilities. Hence, Andelic N et al. analyzed a subgroup of patients from CENTER-TBI with functional disability who needing rehabilitation. The aims consisted of:
- Appraisal of the necessity and allocation of rehabilitation for disabled European TBI patients during the first 6 months post-injury,
- Identification of sociodemographics, comorbidities, and injury-related factors as possible predicting factors for the allocation of rehabilitation.
The CENTER-TBI project was a prospective observational longitudinal study conducted in 18 countries between 2014 and 2017, with participants included based on a diagnosis of TBI, indication for CT scan, and arrival to hospital in the first 24 hours post brain injury.
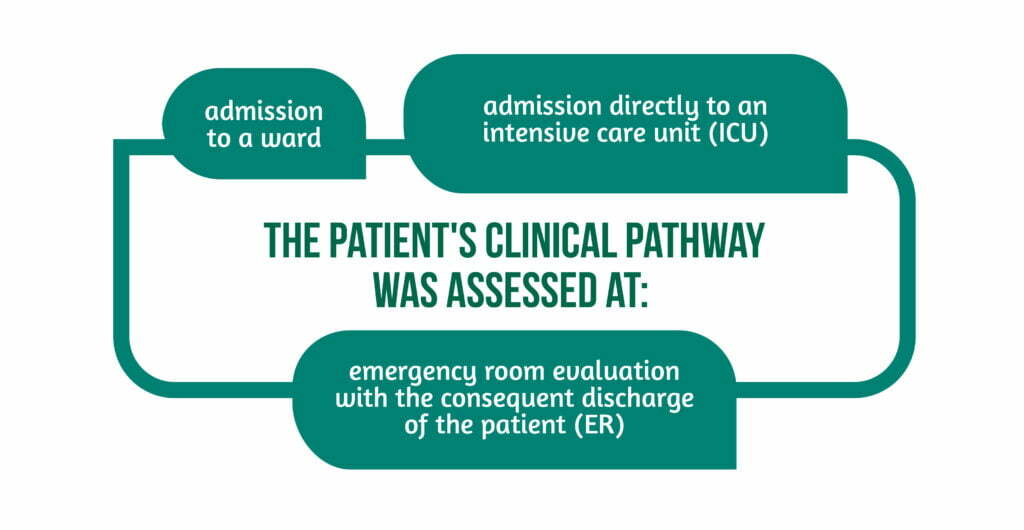
The patient’s clinical pathway was assessed using three levels of care, as showcased in Figure 1.
Methodology
One thousand two hundred six participants aged 16 and above were included, originating from 17 European countries. Individuals had suffered moderate to severe disability post-TBI as measured with the GOSE score at 6 months combined with a GOSE questionnaire reported by patients or their relatives. The resulting scores were collected electronically, combined, and integrated into the database. One crucial aspect mentioned is that the vegetative state and lower severity disability were grouped. In addition, individuals with lower-severe to upper-moderate dysfunctions and thus affected outcomes who provided information about rehabilitation were included in the regression study (512 people) [1].
Data was collected on:
- Sociodemographic characteristics (sex, age, living situation, educational years, employment status)
- Health condition (by categorization of the American Society of Anesthesiologists Physical Status Classification System in healthy, mild or severe systemic disorder and life-threatening severe systemic disorder)
- Injury characteristics (mechanism, pathway of care, severity within 24 hours of TBI, intracranial lesions on CT scan, Abbreviated Injury Scale, Injury Severity Score)
- Geographical region (according to the EU Vocabularies – EuroVoc)
- Various rehabilitation needs according to five established patient’s outcomes (daily life activities measured using QOLIBRI with a threshold for the presence of disability<60 points, physical disability and speech or language disorder, covered by using the CENTER-TBI Participant Questionnaire with yes or no answers, cognitive disorder using part of the Rivermead Post-Concussion Symptoms Questionnaire and psychological disorder considering post-traumatic stress disorder, depression and anxiety as impairments) (Table 1) [1].
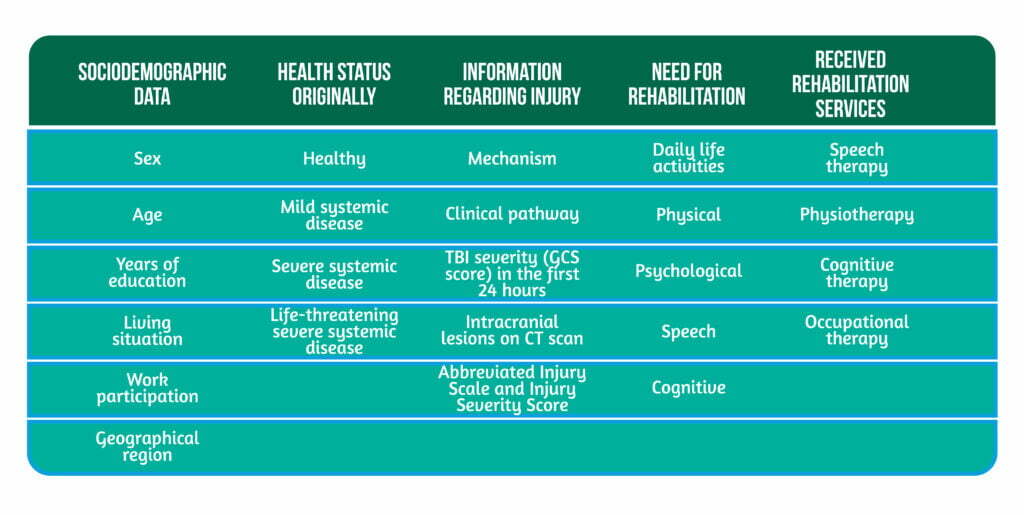
Participants also self-reported the professional aid, and rehabilitation received post-TBI, including:
- cognitive
- physical
- speech
- psychological therapy.
Consequently, patients communicated whether rehabilitation was undertaken and the type of rehabilitation (inpatient, at-home, outpatient, or community-level rehabilitation) [1].
Statistical analysis was used to establish the needs of rehabilitation that were not and to predict the likelihood of receiving rehabilitation. The degree of rehabilitation and professional aid was highlighted by comparing the total number of impaired participants with those who received rehabilitation, thus revealing the portion with unmet need for rehabilitation [1].
The unsatisfied need for rehabilitation was categorized as honored (>75% of participants receiving rehabilitation), almost honored (between 75-25% of patients receiving rehabilitation), and unmet (<25% of participants receiving rehabilitation). Furthermore, the coverage was grouped by the outcome categories mentioned above and then ranked at 3- and 6 months post-TBI. Finally, predicting the likelihood of receiving rehabilitation was done by considering the previous variables (sociodemographic, geographical region, health status before TBI, injury characteristics, TBI severity, and general lesion severity).
Results of the study
The study population comprised of over 65% males within the age group of ~49 years, with half of the population having over 12 years of education, employed, and originally from western European countries. Road traffic accidents represented the most frequent cause of TBI. Post-TBI, two thirds of patients were admitted to the intensive care unit stratum, and over 60% had lesions on CT scan. Additionally, over half of the studied population had no prior health problems.
Regarding the need for rehabilitation, in this study by Angelic Nada et al., over 90% of participants had a reduced outcome (one of the five mentioned above) at 3 months and almost 90% at 6 months. Further, around 40% had a reduced outcome in two or three and ~9% in all five studied outcomes. Interestingly, at 3 months, the physical disabilities represented the primary concern, while at 6 months, these were replaced by the cognitive disabilities. All the other analyzed outcomes had a similar scattering, with language and speech disabilities having the lowest recurrence and the most significant disability being encountered in patients admitted, to begin with, to the intensive care unit. Similar to the identified need, the rehabilitation types provided at 3 and 6 months were according to frequency: physiotherapy, speech, and occupational therapy. About one-third of participants reported the accomplishment of cognitive therapy at 3 and six months.
Nevertheless, less than one-third of patients received professional psychological aid, although reporting disability. Inpatient rehabilitation was primarily done for patients from the ICU stratum, while outpatient rehabilitation was done mainly by patients from the other two strata (ER and ward). Although rehabilitation needs were partly covered (according to the established outcomes), a difference in the ranking was identified between occupational (increased frequency at 3 months post-TBI) and speech therapy (increased frequency at 6 months). Unfortunately, therapy for psychological disability was ranked last, regardless of the post-TBI period.
Almost one-third of participants received inpatient rehabilitation and half as much outpatient rehabilitation, regardless of the disabilities. Mirroring the severity of TBI, patients from the ICU stratum had a higher rehabilitation rate compared to the other strata (ER, ward). Additionally, under 15% of patients from the ICU stratum received outpatient rehabilitation. Missing data for the ICU stratum regarding rehabilitation was up to one-third of the total of patients, mainly those with a lower GOSE score, mirroring a lesser chance for recovery and, consequently, outpatient rehabilitation [1].
The model for predicting the likelihood of rehabilitation post-TBI revealed that TBI severity, physical and cognitive impairment, but no psychological impairment promoted access to rehabilitation, regardless of post-TBI period (3 and 6 months). The ISS and strata did not lead to significant results, but overall, the model successfully predicted the likelihood of rehabilitation for those who received it [1].
Conclusion of the study
This CENTER-TBI study emphasized the unsatisfied need for rehabilitation of patients with moderate to severe TBI, considering their impairments, ranging from physical to cognitive, daily life activities, speech, and psychological disorders, thus confirming the first hypothesis of the study. Additionally, the authors raised an essential question regarding the allocation of post-TBI rehabilitation, secondary to the fact that physical therapy remains the most frequently used rehabilitation type. However, cognitive impairments are the most frequently encountered. Indeed, as the authors mentioned, accessibility to rehabilitation facilities and healthcare systems has to be considered. Last but not least, geographical regions, sex, or age were not predictors of undergoing rehabilitation, contrasting the second hypothesis [1].
Finally, the need for a more comprehensive and standardized assessment of TBI patients has to be done post-injury to allow a proper and in-time selection of rehabilitation, with the goal being improving their outcomes. The assessment should be done on many levels, beginning with patient reports, healthcare professionals to the administrative part, and healthcare systems to ensure a proper acquaintance of the need for TBI rehabilitation [1].
References
- Andelic N, Røe C, Tenovuo O, Azouvi et al. Unmet Rehabilitation Needs after Traumatic Brain Injury across Europe: Results from the CENTER-TBI Study. Journal of clinical medicine 2021, 10(5), 1035. doi: 10.3390/jcm10051035
- Cole WR & Bailie JM. Neurocognitive and Psychiatric Symptoms following Mild Traumatic Brain Injury. In D. Laskowitz (Eds.) et al., Translational Research in Traumatic Brain Injury 2016. CRC Press/Taylor and Francis Group. Available at: https://pubmed.ncbi.nlm.nih.gov/26583174/
- Jourdan C, Bayen E, Bosserelle, V, Azerad et al. Referral to rehabilitation after severe traumatic brain injury: results from the PariS-TBI Study. Neurorehabilitation and neural repair 2013, 27(1), 35–44. doi: 10.1177/1545968312440744.
- Schumacher R, Walder B, Delhumeau C, & Müri RM. Predictors of inpatient (neuro)rehabilitation after acute care of severe traumatic brain injury: An epidemiological study. Brain injury 2016, 30(10), 1186–1193. doi: 10.1080/02699052.2016.1183821.
- Fleminger S & Ponsford J. Long term outcome after traumatic brain injury. BMJ (Clinical research ed.) 2005, 331(7530), 1419–1420. doi: 10.1136/bmj.331.7530.1419




