Keywords: TBI and substance abuse, TBI and substance misuse, TBI and alcohol use, signs of substance abuse, TBi disability, drug overdose,
Focus Keyword: TBI and substance abuse
What is the relationship between TBI and substance abuse?
Substance use disorders or substance abuse and TBI can often occur at the same time. Therefore, it is essential to know their interrelation. People with a history of alcohol use disorder or misuse of other substances have a higher risk of sustaining a TBI. Thus, populations with these affections represent a significant proportion of TBI patients, mainly due to motor, cognitive, and mental impairment secondary to substance abuse. People who sustain a TBI also have a higher incidence of substance misuse before and after the injury. TBI will result in a broad category of disabilities (physical, psychological, cognitive) [1–4].
Misuse of substances (alcohol and other drugs) will challenge the rehabilitation process and impact the chance of a favorable treatment following TBI. Unfortunately, compared to alcohol consumption, the relation between TBI and abuse of other substances has been less explored [3].
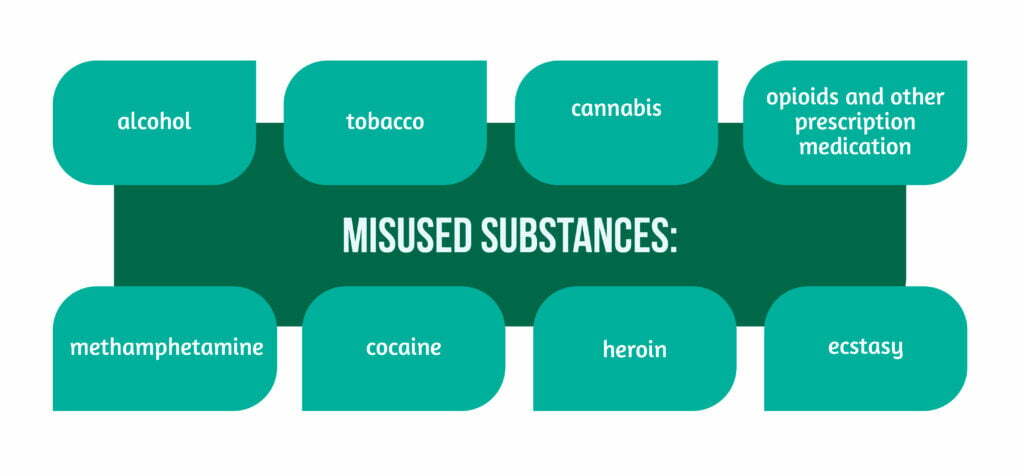
Substance misuse is defined as the inefficient use of a substance that, due to the frequency of administration, amount consumed, or situation in which it is consumed, is harmful to an individual or those around them, leading to injury.
Some examples are showcased in Figure 1 [5].
It is essential to consider and assess the risk associated with the misuse of substances before and after TBI, due to various aspects:
- Behavioral impact (aggressiveness, confrontational behavior)
- Cognitive changes (mental impairment)
- Damaged motor control
- Comorbidities
- Previous misuse of substances [2,3].
Additionally, substance use tends to decrease or even stop in the early period after TBI. A significant number of users not only restart their consumption, but also increase it about one year after TBI and maintain the habit in the long term. For these patients, a critical shaping factor is represented by their environment, namely the caregivers, having continuous supervision and limited access to the substance, or institutionalization. Furthermore, individuals with a history of substance abuse are at higher risk of post-TBI continuation of the habit than those without a history [2].
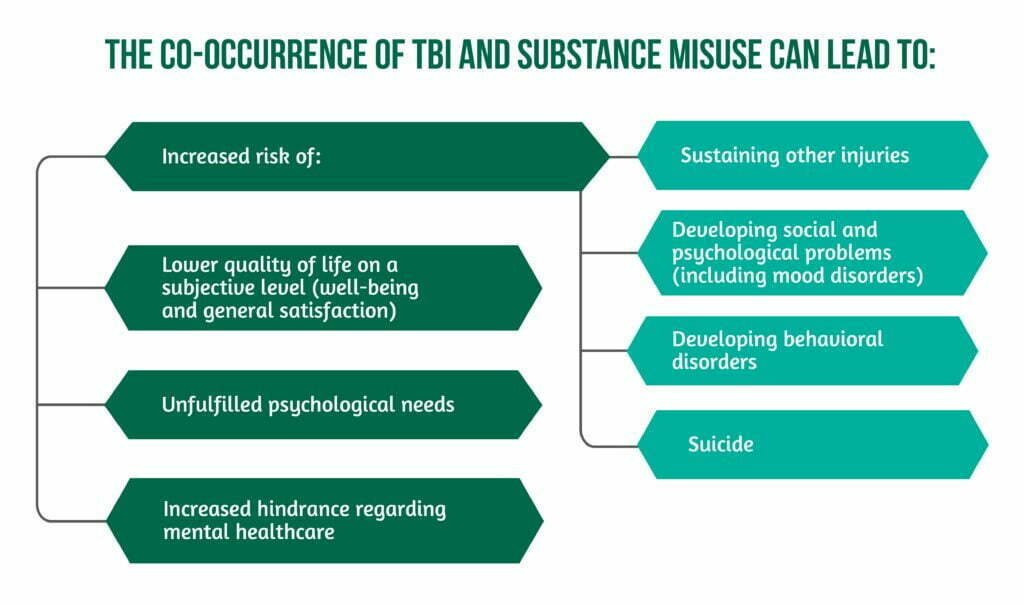
Furthermore, the co-occurrence of TBI and substance misuse has shown to lead to [2]:
Moreover, there is a correlation between alcohol consumption and the misuse of other substances.
Behavioral changes after TBI (disability changes in executive functions, disinhibition, or impulsivity) represent a contribution to the development of the disorder. This is one of the reasons why the presence of both TBI and substance misuse requires the evaluation of the behavioral changes, especially regarding risk-taking [2].
Case reports showcase a significant influence of several substances on the behavior of the individual consuming them:
- Fatal TBI after attempting to do “car surfing” (in the context of MDMA consumption)
- Damage at the level of the frontal lobe (in the context of amphetamine consumption)
- TBI-proneness (e.g., the case of Ernest Hemingway) [3].
Did you know?
Ernest Hemingway, the Nobel Prize for literature winner for his world-renowned “The Old Man And The Sea” repeatedly suffered from TBIs during his tumultuous lifetime. He played football and boxed, suffered concussions during World War II, suffered a car accident and a motorcycle accident which projected his head into a rock, accidentally fell from his boat leading to a concussion, and survived a plane crash from which he suffered a skull fracture. It was reported that all of these have led to him suffering from Chronic Traumatic Encephalopathy. Unfortunately, he also suffered from psychiatric disorders leading to his suicide [6].
The use of marijuana, methamphetamine, cocaine, and prescription medication (e.g. benzodiazepines for anxiety or opioids like oxycodone and OxyContin for pain management) can lead to all the symptoms mentioned above, as well as overlap with most effects that also appear as a result of Alcohol consumption. Additionally, combining these substances will further increase the risk of substance addiction, even overdose [1]. Opiates are frequently used for pain management in TBI patients, but the physician considers the risk-benefit before recommending the treatment [3].
The use of alcohol together with pain or anxiety medication can be deadly [1]!
What should be done in cases of substance abuse and TBI?
The priority of TBI patients is the prevention of secondary lesions post-TBI and assurance of care. Usually, patients undergo screenings (to identify the substance), clinical interviews, questionnaires, and physical examinations [2,4].
Elements that help in identifying an individual with substance addiction are:
- Verbal referencing to substance misuse (e.g., feeling guilty because of the use, depreciation, negation of the use)
- Social activities related to substance misuse
- Improper educational or vocational activities (tardiness, frequent changes in vocation, absences)
- Irritability when asked about substance use
- Focus on substance-related issues [4].
Identifying elements associated with a higher risk of developing post-TBI substance abuse:
- Substance abuse before TBI
- Intoxication at time of the TBI
- History of illegal activities due to substance misuse
- Age under 25 years
- Unawareness or ignorance of the effects of substance abuse [4].
How can society offer help for the prevention, treatment, and rehabilitation in the case of substance abuse?
First and foremost, an important factor is educating the patient and relatives regarding the prevention and treatment of substance abuse, ranging from risk factors and the signs of abuse, to methods of treatment. Family members’ involvement is of utmost importance since most TBI patients will resume living together with their loved ones after a TBI. Therefore, the family has an essential role in the care of the injured person.
Simultaneously and equally important is to educate the patient and caregivers about the signs and symptoms associated with substance abuse and those associated with TBI individually, also underlining their impact on the patient and his disability. Motivational counselling can emphasize the advantages and disadvantages of substance abuse while also using different strategies for helping the patients understand, manage, and carry on with the encountered difficulties [2,4].
Referrals for different support groups represent another effective intervention (e.g., Alcoholics Anonymous or Narcotics Anonymous).
Generally, the rehabilitation of patients is a multidisciplinary pursuit, involving a combination of interventions covering disability on a cognitive, emotional, social, and physical level, as well as reintegration into society with engagement in several activities (including work) [2–4].
How about drug overdose?
One important aspect regarding the misuse of substances is the danger of overdosing. With increasing drug-related mortality during the past years, the pandemic times probably led to a further increase, by directly affecting in-person group meetings, access to medical and mental care, and increasing anxiety by impacting housing, employment, etc. Social distancing for an addict meant being alone, including at the moment of overdose or TBI, consequently with no one near to offer help.
Nonetheless, many overdoses can be overcomed. Unfortunately, substance abusers often avoid presenting to healthcare facilities due to shame and desire to avoid judgment from others, as well as due to the use of illicit substances and poor care received.
One positive aspect regarding the criminalization of substance abuse is the “Good Samaritan Law” from Maryland, US, which states that individuals that are having or helping during an overdose will receive protection from being arrested, prosecuted, or charged with possession of a controlled dangerous substance or equipment. All this is to encourage patients to present to healthcare facilities in case of overdose [7].
Conclusion
The aim of addressing and emphasizing the interrelation of TBI and substance abuse with its consequences and possible therapies is the improvement of functional independence and overall quality of life by reducing the attached disability. To have an optimal recovery after TBI, during the rehabilitation process, substance misuse needs to be identified and treated [2-4]. Additionally, the impact of TBI and substance abuse has a comprehensive representation as it has been emphasized in Alcohol consumption and TBI: a continuing problem for patients and society?
Finally, substance misuse can stop or hinder the rehabilitation process after TBI, and TBI will make people more vulnerable to the effects of these substances, with the risk of endangering their lives [1–7].
To learn more about the impact of TBIs, visit:
- Can TBI affect balance?
- What should you do when experiencing post-TBI seizures?
- Can TBI affect emotions and behaviors?
- Fatigue frequency after TBI
References
- Bombardier CH, and Corrigan JD in collaboration with the American Institutes for Research Model Systems Knowledge Translation Center. Alcohol use after traumatic brain injury, Model Systems Knowledge Translation Center, 2021. Available at: https://msktc.org/tbi/factsheets
- Olson-Madden, JH, Brenner, LA, Corrigan, JD, Emrick CD & Britton PC. Substance use and mild traumatic brain injury risk reduction and prevention: a novel model for treatment. Rehabilitation research and practice 2012, 174579. DOI: 10.1155/2012/174579
- Graham, DP & Cardon AL. An update on substance use and treatment following traumatic brain injury. Annals of the New York Academy of Sciences 2008. DOI: 10.1196/annals.1441.029
- Taylor LA, Kreutzer JS, Demm SR, & Meade MA. Traumatic brain injury and substance abuse: A review and analysis of the literature. Neuropsychological rehabilitation 2003. https://doi.org/10.1080/09602010244000336
- Brain Injury Canada, Substance use, c:2022, available at: https://braininjurycanada.ca/en/living-brain-injury/substance-use/
- Kemper Campbell J., Did Chronic Traumatic Encephalopathy Contribute to Ernest Hemingway’s Death?, American Academy of Ophtalmology, 2017, June 9, c: American Academy of Ophtalmology 2022. Available at: https://www.aao.org/senior-ophthalmologists/scope/article/did-concussions-contribute-to-hemingways-death
- Bartolomei-Hill L, Edmonston A, Maryland Traumatic Brain Injury Partner Grant. Uncovering the Connection The relationship between opioids and brain injury, harm reduction strategies through a Brain Injury Informed Lens, Maryland Department of Health 2020. Available at: https://health.maryland.gov/bha/Documents/Brain%20Injury%20%20Harm%20Reduction%20Strategies.pdf




